This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
proofread
Understanding the role of neurofilament light chain in MS and other neurological conditions
The human body is an intricate network of systems, and central to its operation is the central nervous system (CNS), consisting of the brain and spinal cord—serving as the main command center.
Understanding the CNS and its malfunctions is a critical part of medical science, and one way we do this is through the use of biomarkers—measurable indicators. Biomarkers can be described as biological "signals" indicating the presence or progression of a disease. In the context of CNS diseases, one such biomarker that has been gaining prominence is the neurofilament light chain (NfL).
Mulitple sclerosis and new biomarkers—NfLs
Multiple sclerosis (MS) is a long-term disease that affects the brain and spinal cord. It's caused by an overactive immune system that mistakenly attacks healthy parts of the body, leading to damage to the protective layer around nerve fibers. This is what experts call a "demyelinating disease."
MS can present itself in different ways. In most people (around 85%), the disease comes and goes, with periods of relative health in between episodes of symptoms—this is known as relapsing-remitting MS. However, for about 15% of people with MS, the disease gets progressively worse from the start without any periods of remission. This is referred to as progressive MS, which can be either primary or secondary.
At the core of MS lies two destructive forces: oxidative stress, which is like a form of "rusting" in the body, and inflammation of the nerve tissue, often a reaction to the body fighting off perceived threats.
Both of these forces are significant players in the development and progression of MS. Unfortunately, these processes ultimately lead to unavoidable damage to the nerve fibers or "axons," which are essential for carrying electrical signals around the body. Understanding these processes helps us grasp the complex nature of this disease.
Neurofilament light chain (NfL) is a key building block in the "wires" of your brain, which are known as axons. These axons help transmit messages, just like wires transmit electricity. Usually, these axons contain a lot of NfL, and only a tiny bit of NfL is "leaked" out. As we get older, a bit more NfL might leak out, but generally, it stays mostly inside the axons. However, when these axons get damaged, through diseases or injury, they can leak a lot more NfL.
This leaked NfL can then find its way into the brain's "cushioning fluid," known as cerebrospinal fluid (CSF), which is the fluid that surrounds and protects the brain and spinal cord. From there, it can move into the bloodstream. But remember, the amount of NfL in the blood is a lot less than in the cerebrospinal fluid.
Since NfL might give clues about these diseases, more and more scientists are studying it. Even though the cerebrospinal fluid might give us more accurate information, it's much easier to take a blood sample. This is why there's a lot of interest in finding easy and accurate ways to measure NfL levels in the blood.
SIMOA: A reliable method for biomarker detection
Research by Burak Arslan and Aylin Sepici Dinçel, from the Department of Medical Biochemistry, Gazi University Faculty of Medicine, Ankara, Turkey, has shown something more—the role of NfLs in non-demyelinating CNS diseases.
The research process involved gathering CSF and blood samples from patients suffering from various CNS diseases, both demyelinating and non-demyelinating. For the accurate and sensitive measurements, authors utilized an innovative technique called the Single Molecule Array (SIMOA) method. SIMOA is renowned for its ability to detect minute amounts of substances in biological samples, making it an ideal tool to quantify NfL levels.
The results showed that NfL levels in CSF could serve as an effective tool not only for tracking demyelinating diseases, but also for managing non-demyelinating CNS diseases. The research has been published in the Bosnian Journal of Basic Medical Sciences.
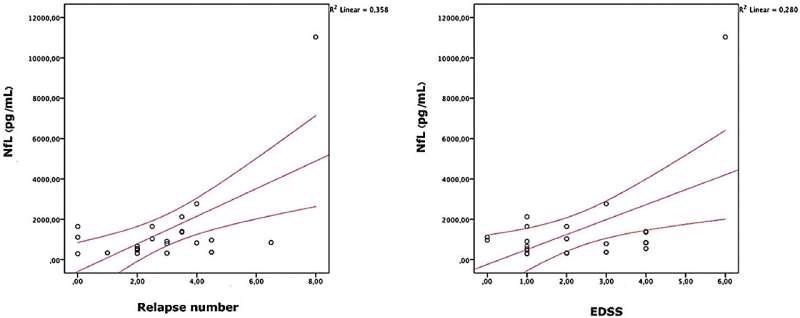
One of the significant observations was that patients with malignant brain tumors presented higher NfL levels. Additionally, authors found a strong correlation between the number of T2 lesions (a specific type of abnormality visible in brain scans) in patients with multiple sclerosis and their CSF NfL levels.
On the technical side, this study confirmed the superiority of the SIMOA method for measuring NfL levels in the blood compared to conventional methods. This finding reinforces the value of SIMOA as a trusted technique for sensitive detection of biomarkers, enhancing its potential for wider adoption in clinical practice.
However, scientific pursuit is never-ending. This study, while offering vital insights, was restricted by its small size and the inherent limitations of research funding and ethical considerations related to biological sample collection. Hence, to delve deeper into the role of NfL levels in non-demyelinating CNS diseases, more extensive studies are required.
In summary, this research adds a piece to the puzzle of understanding CNS diseases. We have known about the potential of NfL as a biomarker for demyelinating diseases, but this study opens up new avenues for its use in non-demyelinating conditions as well.
Furthermore, these findings reaffirm the reliability and robustness of the SIMOA method for these investigations. The quest for understanding is far from over, and further research is needed to draw a comprehensive picture.
More information: Burak Arslan et al, Evaluation of cerebrospinal fluid neurofilament light chain levels in multiple sclerosis and non-demyelinating diseases of the central nervous system: clinical and biochemical perspective, Bosnian Journal of Basic Medical Sciences (2022). DOI: 10.17305/bjbms.2021.7326

















