This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
written by researcher(s)
proofread
One in six women are diagnosed with gestational diabetes. But this diagnosis may not benefit them or their babies
When Sophie was pregnant with her first baby, she had an oral glucose tolerance blood test. A few days later, the hospital phoned telling her she had gestational diabetes.
Despite having only a slightly raised glucose (blood sugar) level, Sophie describes being diagnosed as affecting her pregnancy tremendously. She tested her blood glucose levels four times a day, kept food diaries and had extra appointments with doctors and dietitians.
She was advised to have an induction because of the risk of having a large baby. At 39 weeks her son was born, weighing a very average 3.5kg. But he was separated from Sophie for four hours so his glucose levels could be monitored.
Sophie is not alone. About one in six pregnant women in Australia are now diagnosed with gestational diabetes.
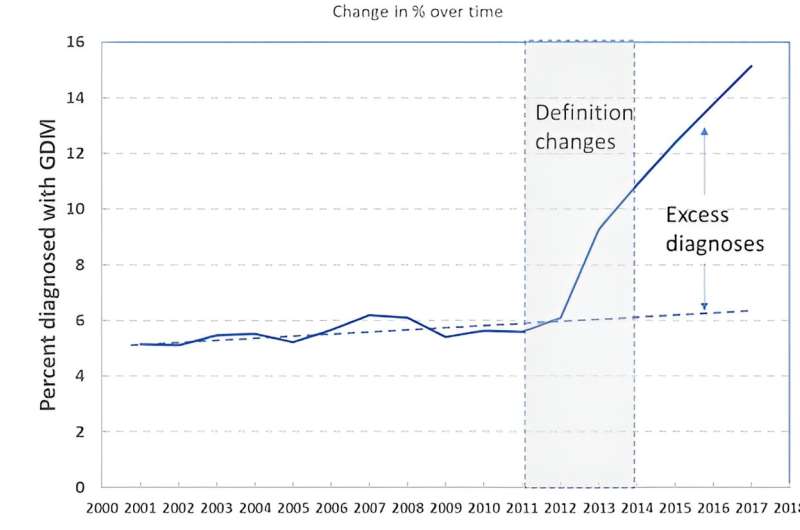
That was not always so. New criteria were developed in 2010 which dropped an initial screening test and lowered the diagnostic set-points. Gestational diabetes diagnoses have since more than doubled.
But recent studies cast doubt on the ways we diagnose and manage gestational diabetes, especially for women like Sophie with only mildly elevated glucose. Here's what's wrong with gestational diabetes screening.
The glucose test is unreliable
The test used to diagnose gestational diabetes—the oral glucose tolerance test—has poor reproducibility. This means subsequent tests may give a different result.
In a recent Australian trial of earlier testing in pregnancy, one-third of the women initially classified as having gestational diabetes (but neither told nor treated) did not have gestational diabetes when retested later in pregnancy. That is a problem.
Usually when a test has poor reproducibility—for example, blood pressure or cholesterol—we repeat the test to confirm before making a diagnosis.
Much of the increase in the incidence of gestational diabetes after the introduction of new diagnostic criteria was due to the switch from using two tests to only using a single test for diagnosis.
The thresholds are too low
Despite little evidence of benefit for either women or babies, the current Australian criteria diagnose women with only mildly abnormal results as having "gestational diabetes."
Recent studies have shown this doesn't benefit women and may cause harms. A New Zealand trial of more than 4,000 women randomly assigned women to be assessed based on the current Australian thresholds or to higher threshold levels (similar to the pre-2010 criteria).
The trial found no additional benefit from using the current low threshold levels, with overall no difference in the proportion of infants born large for gestational age.
However, the trial found several harms, including more neonatal hypoglycemia (low blood sugar in newborns), induction of labor, use of diabetic medications including insulin injections, and use of health services.
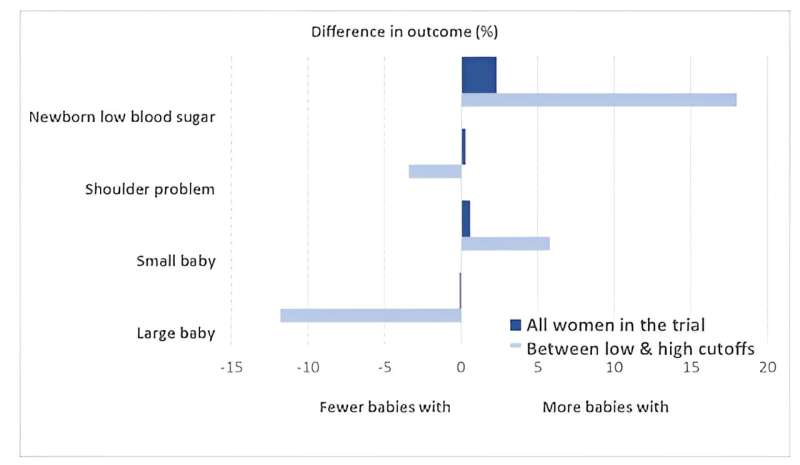
The study authors also looked at the subgroup of women who were diagnosed with glucose levels between the higher and lower thresholds. In this subgroup, there was some reduction in large babies, and in shoulder problems at delivery.
But there was also an increase in small babies. This is of concern because being small for gestational age can also have consequences for babies, including long-term health consequences.
Testing too early
Some centers have begun testing women at higher risk of gestational diabetes earlier in the pregnancy (between 12 and 20 weeks).
However, a recent trial showed no clear benefit compared with testing at the usual 24–28 weeks: possibly fewer large babies, but again matched by more small babies.
There was a reduction in transient "respiratory distress"—needing extra oxygen for a few hours—but not in serious clinical events.
Impact on women with gestational diabetes
For women diagnosed using the higher glucose thresholds, dietary advice, glucose monitoring and, where necessary, insulin therapy has been shown to reduce complications during delivery and the post-natal period.
However, current models of care can also cause harm. Women with gestational diabetes are often denied their preferred model of care—for example, midwifery continuity of caregiver. In rural areas, they may have to transfer to a larger hospital, requiring longer travel to antenatal visits and moving to a larger center for their birth—away from their families and support networks for several weeks.
Women say the diagnosis often dominates their antenatal care and their whole experience of pregnancy, reducing time for other issues or concerns.
Women from culturally and linguistically diverse communities find it difficult to reconcile the advice given about diet and exercise with their own cultural practices and beliefs about pregnancy.
Some women with gestational diabetes become extremely anxious about their eating and undertake extensive calorie restrictions or disordered eating habits.
Time to reassess the advice
Recent evidence from both randomized controlled trials and from qualitative studies with women diagnosed with gestational diabetes suggest we need to reassess how we currently diagnose and manage gestational diabetes, particularly for women with only slightly elevated levels.
It is time for a review to consider all the problems described above. This review should include the views of all those impacted by these decisions: women in childbearing years, and the GPs, dietitians, diabetes educators, midwives and obstetricians who care for them.
This article is republished from The Conversation under a Creative Commons license. Read the original article.![]()





















