This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Comprehensive insulin signaling map shows interplay between genes and diet
Researchers have produced a comprehensive picture of insulin signaling in mice and suggest that it is shaped by entangled effects of genetics and diet.
The research, published today as a Reviewed Preprint in eLife, is described by the editors as a fundamental study of substantial importance. They say the authors share compelling evidence that sheds light on the interplay between genetic attributes and environmental conditions in shaping insulin signaling in skeletal muscle—a crucial regulator of metabolism.
The study also provides a unique tool for assessing the range of phosphorylation in insulin reactions and is anticipated to provide inspiration for further research into metabolic disease and diabetes.
"Insulin resistance—the failure of insulin to promote glucose uptake in its target tissues—is triggered by genetic and environmental factors such as family history and high-calorie diets," says lead author Julian van Gerwen, during the study an undergraduate at the School of Life and Environmental Sciences, University of Sydney, Australia. "Although insulin resistance is a major precursor of metabolic disease, including type 2 diabetes, its mechanistic basis remains unresolved."
Insulin normally tells the body to absorb glucose (sugar) from the bloodstream via a complex and dynamic signaling pathway. These signals are enabled by a process called phosphorylation—the addition of a phosphate group to a protein at a very specific position (called a phosphosite).
It is thought that insulin signaling controls thousands of phosphosites, but many are still uncharacterized. In addition, although it is well known that individual people vary greatly in their physiological response to insulin, it remains unclear how genetics or diet influence the phosphorylation status of cellular proteins—also known as the phosphoproteome.
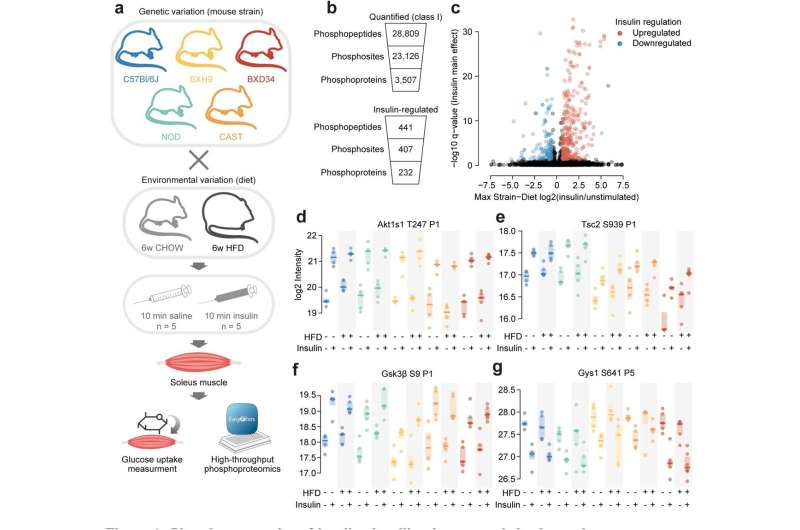
To address this, van Gerwen and colleagues studied mice with well-characterized but different genetic backgrounds, so they could decipher the specific effects of genetics and diet on insulin signaling.
They fed five strains of mice either a normal or high-fat and high-sugar diet, and took samples of their skeletal muscle—the site of greatest insulin-triggered glucose uptake after eating. Then they measured phosphorylation of the thousands of proteins present in each muscle sample using mass spectrometry. Their analysis recovered many well-known insulin-regulated phosphosites, and many more novel sites that had not previously been associated with insulin signaling.
To explore the influence of genetic and environmental variation, the team developed an algorithm to analyze which changes could be attributed to genetics, diet, or their combination. Almost half of all insulin-regulated phosphosites were affected by the strain of the mice when fed a normal diet, either having a stronger or weaker response to insulin. Overall, each genetic background displayed a unique fingerprint of insulin signaling.
By contrast, although there were changes in insulin signaling caused by diet, the vast majority of these were shaped by the genetic background of the mice. Many phosphosites even changed in the opposite direction between multiple strains, highlighting that the molecular impacts of a high-fat diet are strongly controlled by genetics.
To explore whether these changes in phosphorylation amounted to an altered insulin response in the mice, the team also measured glucose uptake in the same muscles used for the phosphoproteome analysis. By linking all insulin-regulated phosphosites with the level of glucose uptake, the researchers narrowed down on a set of key phosphosites likely to control the insulin response. Inspired by one of these phosphosites, the team found that modulating a specific protein could reverse insulin resistance in a cell-based model.
The authors point out that the genetic and diet-driven changes in phosphorylation largely could not be predicted by the current model of the insulin signaling pathway. This highlights that our knowledge of this pathway is far from complete, and they say that the next step is to investigate underlying biomolecular mechanisms that could link common changes. They also suggest that incorporating female mice and a wider range of genetic backgrounds will strengthen their research.
"The protein phosphorylation landscape is vast and intricate, akin to a night sky filled with stars," explains senior author David James, a professor at the School of Life and Environmental Sciences and Faculty of Medicine and Health, University of Sydney. "Many teams have sought to organize these stars into constellations and chart those that collapse in disease. However, most have only used cell lines and lab animals of limited genetic backgrounds."
"In this study, when we examined genetic and environmental variation—as occurs in the human population—we observed a complete rearrangement of the night sky, marked by a fading of the familiar constellations and the emergence of entirely new galaxies. To truly comprehend how diseases manifest from signaling aberrations, we must adapt to this newfound complexity. Our work provides a launching pad for future studies to tackle this complexity for insulin resistance and diabetes."
More information: Julian van Gerwen et al, The genetic and dietary landscape of the muscle insulin signalling network, eLife (2023). DOI: 10.7554/eLife.89212.1 elifesciences.org/reviewed-preprints/89212

















