This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Why is the brain so prone to inflammation?
All living cells teem with ribonucleic acid (RNA), molecules that relay genetic messages to keep cells functioning. But these necessary molecules can also set off cellular alarms. The long twisted-together strands of RNA in viruses, for instance, are a tell-tale sign of an invader and the human immune system triggers inflammation in their presence.
Early in her research career, Hachung Chung, Ph.D., wondered how the immune system could tell the difference between disease-causing viral RNA and our own normal RNA. Now, that question has led her research in a surprising direction—the study of brain diseases including Alzheimer's, amyotrophic lateral sclerosis (ALS) and lupus brain fog. Chung's latest results suggest that the incorrect sensing of our own RNA in the brain may be to blame for chronic inflammation in conditions like these.
"I think neurodegenerative diseases are the last frontier of biomedicine where development of therapeutics has been confounding and slow," says Chung, assistant professor of microbiology & immunology in the Vagelos College of Physicians and Surgeons. "I think for many of these diseases, if we can harness the immune system in the right way, we might see a breakthrough."
The convergence of immunology and brain science
Scientists have long known that immune molecules responsible for recognizing viruses, known as pattern recognition receptors, can detect viral double-stranded RNA structures, which form when two complementary RNA strands bond together.
As a postdoctoral fellow, Chung initially studied if the RNA modifying enzyme ADAR1 could target viral dsRNAs and alter the course of viral infection. Around the same time, however, another researcher discovered that mutations disrupting the function of ADAR1 cause the autoimmune disease Aicardi-Goutières syndrome (AGS), in which the immune system attacks healthy brain cells.
Those surprise findings suggested that ADAR1 was not only important in viral infection but was critical for keeping biological peace in the body in other ways.
"I thought it was really interesting that not having this RNA editing protein would suddenly cause such severe symptoms in the brain, even when there was no virus around," Chung recalls. "It made me really curious what the protein is doing to keep us healthy separately from its role in virus infection."
Chung, then working with mentor Charles Rice at Rockefeller University, discovered that ADAR1-mediated modifications made to our own double-stranded RNA molecules keep pattern recognition receptors from constantly triggering inflammation in healthy tissues. The team reported their findings in Cell in 2018.
That finding satisfied some of Chung's curiosity about how pattern recognition receptors avoid flagging healthy human RNA, but questions still abounded.
"We still don't know exactly how ADAR1 works to hide human RNA from pattern recognition receptors," Chung says. "We think that it might make a little kink in the RNA duplex, making it harder to find by pattern recognition receptors."
Chung's research into ADAR1 persisted when she launched her own research lab at Columbia in 2019. She wanted to find out why the symptoms of AGS were mostly in the brain, when RNA is found throughout the body. If mutations in ADAR1 make the immune system recognize RNA in the brain and trigger inflammation, why didn't it also cause similarly high levels of inflammation in the heart, the liver, the blood and elsewhere?
Triggering brain inflammation
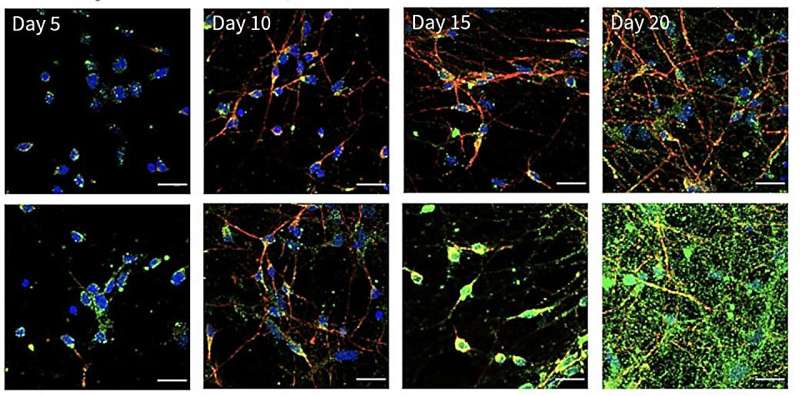
In her latest study, published in Science Immunology in October 2023, two members of the Chung lab, Tyler Dorrity, Ph.D., and Heegwon Shin, Ph.D., engineered stem cells to lack ADAR1 and then coaxed both normal stem cells and those without ADAR1 to develop into neurons and other cell types. They discovered that neurons, compared to other cells, have far more long double-stranded RNA structures like that found in viruses.
Without ADAR1, most cells had just small amounts of double-stranded RNA for pattern recognition receptors to flag as dangerous. Neurons, on the other hand, had a lot. Without ADAR1 to disguise the RNA, pattern recognition receptors immediately triggered inflammation in neurons. In turn, that inflammation can increase levels of pattern recognition receptors, exacerbating the response in a difficult-to-stop cycle.
"Once you get this initial spike in inflammation, whether it's due to a virus or to an autoimmune reaction, you can get locked into this loop where pattern recognition receptors keep finding RNA and then you make more pattern recognition receptors," says Chung.
This likely explains what occurs in the brains of people with AGS, but also hints at a possible mechanism for the hard-to-stop inflammation seen in conditions like lupus brain fog, ALS, and Alzheimer's disease.
A constant patrol
To try combating the inflammation in their isolated neurons, Chung's team decreased the levels of free-floating, double-stranded RNA in the cells. While this did decrease inflammation, it also led to another surprise: the neurons suddenly became more susceptible to infections with Zika virus and herpes simplex virus.
"We realized that it's actually important for your neurons to have this low-level inflammation," Chung says.
This minor inflammation triggered by RNA in the brain takes on the role of a pilot light on a stove—it keeps the immune system activated and ready to react more quickly when there is an invading virus, she hypothesizes.
"In textbooks, we've learned that pattern recognition receptors are sitting around waiting for pathogens," says Chung. "But our research is starting to suggest that maybe these molecules are always sensing some of our own RNA and keeping inflammation turned on at a very low level."
Rather than be discouraged by all the surprises in her latest study, Chung is more motivated than ever to understand the complex interplay between RNA and immune responses in the brain—and elsewhere.
"Science is addictive," she says. "I love those humbling moments where your experiment worked but it gave you totally different results than you expected. It just proves that there is so much more to understand."
More information: Tyler J. Dorrity et al, Long 3′UTRs predispose neurons to inflammation by promoting immunostimulatory double-stranded RNA formation, Science Immunology (2023). DOI: 10.1126/sciimmunol.adg2979



















