This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
proofread
Elevated glutamine triggers stroke risk in moyamoya disease via endothelial‐to‐mesenchymal transition, finds study
A study appearing in MedComm has been led by Dr. Jizong Zhao, Dr. Dong Zhang, and Dr. Peicong Ge (Department of Neurosurgery, Beijing Tiantan Hospital, Capital Medical University and Department of Neurosurgery, Beijing Hospital). The team presents a comprehensive investigation involving 360 adult MMD patients, finding that elevated serum glutamine levels were linked to increased stroke risk. Manipulation of integrin subunit beta 4 (ITGB4) and the use of atorvastatin was reported to alleviate the glutamine-induced EndMT, offering potential new therapeutic approaches for MMD.
Despite the severe presentations in MMD, the pathophysiological mechanisms driving MMD remain incompletely understood. The risk of stroke—a common and severe complication of MMD, is a pivotal aspect in reducing the devastating circumstances caused by MMD.
"Our research aimed to explore the role of glutamine in determining stroke risk and identify potential therapeutic targets," said Peicong Ge, the senior researcher of the study.
This study involved an in-depth investigation involving a cohort of 360 adult MMD patients. The researchers found that high glutamine levels were positively correlated with an increased risk of stroke, revealing a greater probability of either hemorrhagic or ischemic stroke as the glutamine concentration rose.
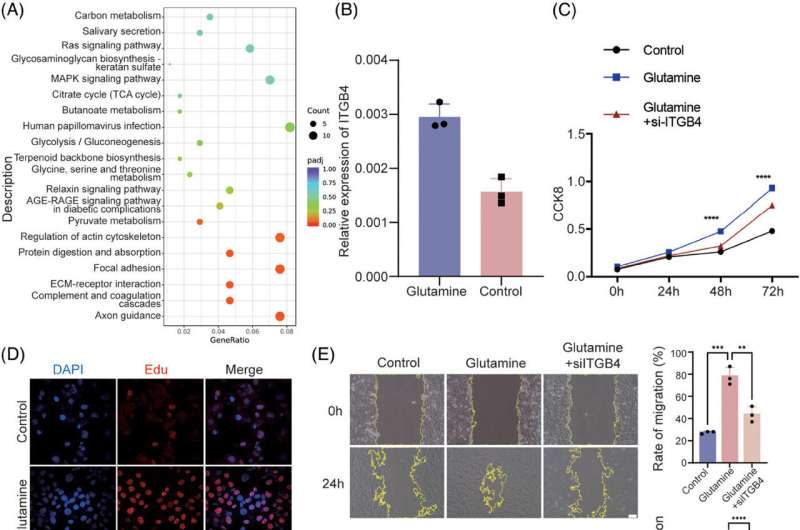
Using human brain microvascular endothelial cells (HBMECs) as a model that accurately replicated the cellular environment of the brain's microvessel, the research team explored the effects of glutamine on these cells. The treatment of HBMEC with glutamine led to notable increases in cell proliferation, migration, and EndMT, illuminating the direct impact of glutamine on endothelial cell behavior.
This provided insight into a potential mechanism by which elevated glutamine levels could lead to the vascular abnormalities observed in MMD.
Crucially, these effects were reversed when the cells were genetically modified to reduce the levels of the protein integrin subunit beta 4 (ITGB4). Further analysis revealed that ITGB4 plays a role in the MAPK-ERK-TGF-β/BMP signaling pathway, which is activated during EndMT.
By targeting Smad4, a protein component of this pathway, the researchers demonstrated that knocking down Smad4 could inhibit the EndMT process. These observations indicate that ITGB4 and the signaling pathway it influences could be promising targets for therapeutic intervention.
In addition to the novel findings related to ITGB4, the study further unveiled the therapeutic potential of atorvastatin, a medication commonly prescribed to lower cholesterol. In lab experiments, atorvastatin was shown to suppress EndMT in ITGB4-transfected HBMECs by inhibiting Smad1/5 phosphorylation and inducing Smad4 ubiquitination, indicating that atorvastatin might offer a new use in treating MMD.
Supporting their laboratory findings, researchers also examined tissue samples from the superficial temporal arteries of MMD patients, confirming that ITGB4 protein levels were indeed upregulated in affected individuals.
"This validation in human tissue is crucial as it bridges the gap between in vitro findings and clinical relevance," Dong Zhang added.
Concluding the study, the researchers point to glutamine as an independent risk factor for hemorrhage or infarction in MMD and suggest that interventions targeting ITGB4 or applying atorvastatin could offer novel therapeutic approaches capable of reducing stroke risk in MMD patients.
"Our findings present a profound opportunity to shift how we approach the treatment of MMD," stated Qiheng He, the first author of the study.
"Beyond potentially using atorvastatin to target specific pathways involved in MMD, one most important thing is that we first clearly reported the phenomenon of EndMT in the endothelium of patients with MMD, which is further related to clinical manifestations, providing a new idea for subsequent research on complex mechanisms of MMD and in revolutionizing the care and treatment of patients."
More information: Qiheng He et al, High glutamine increases stroke risk by inducing the endothelial‐to‐mesenchymal transition in moyamoya disease, MedComm (2024). DOI: 10.1002/mco2.525




















