This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
New study probes macrophages' role in developing pulmonary fibrosis
Scientists have long known that white blood cells called macrophages accumulate in the lungs of people suffering from pulmonary fibrosis. What role macrophages play in developing the often fatal lung disease is less clear.
A new University at Buffalo-led study sheds light on this mystery and opens new paths to study pulmonary fibrosis, advancements that could ultimately lead to more effective medicine and therapies for the disease, which affects roughly 100,000 in the U.S.
"Our understanding of how pulmonary fibrosis develops has greatly improved; however, there is still much we do not understand, especially the involvement of immune cells in the formation of the disease," says the study's corresponding author Ruogang Zhao, Ph.D., associate professor of biomedical engineering at the University at Buffalo.
In people with pulmonary fibrosis, stiff scar tissue forms in the lungs, making it difficult to breath. This stiff scar tissue cannot be repaired, only slowed down with medicine and therapies.
The study, published in Science Advances, describes how Zhao and colleagues developed a miniature models of fibrotic lung tissues that act as a proxy for someone with pulmonary fibrosis.
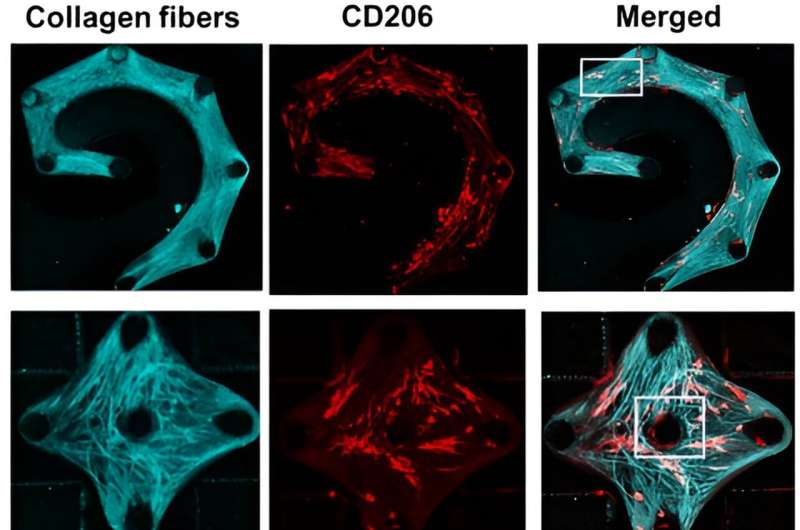
In addition to macrophages, the model included the two main components of stiff scar tissue: fibroblasts and collagen fibers.
During experiments, the team observed macrophages sensing their surroundings and becoming "coaligned" with the fibroblasts and collagen fibers. This activation of the macrophages' mechanical sensitivity allowed them to secrete additional biochemical factors that promote scar tissue growth.
The team then dosed the diseased tissue with a drug called pirfenidone, which is a Food and Drug Administration-approved treatment that slows down the worsening of pulmonary fibrosis. Pirfenidone blocks certain proteins that can significantly affect how macrophages adhere to and interact with fibroblasts and collagen fibers. As a result, the drug can stop scar tissue from forming.
"The results suggest a potential mechanism, at the tissue level and involving macrophages, of how pulmonary fibrosis originates," says the study's first author Ying Xu, a Ph.D. candidate in Zhao's lab.
The fibrotic lung tissue model, Zhao adds, is a powerful new tool that researchers can use to further study tissue- and cell-level interactions in fibrotic lungs. It could also help test new drugs that further slow down the disease or stop it, he says.
More information: Ying Xu et al, Modeling mechanical activation of macrophages during pulmonary fibrogenesis for targeted anti-fibrosis therapy, Science Advances (2024). DOI: 10.1126/sciadv.adj9559


















