This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Targeting 'monster cancer cells' could reduce recurrence rates after cancer therapy
MUSC Hollings Cancer Center researchers have unlocked a discovery that could help to explain why cancer can recur in patients who have undergone chemotherapy or radiotherapy.
Both types of therapy put cancer cells under stress, with the goal of causing them to self-destruct. However, these treatments do not always produce durable cures, as cancer cells adapt to stress, escape and allow the tumor to resurge after a short time.
Recently, scientists have begun to look at the role of polyploid giant cancer cells, or PGCCs, in cancer recurrence. Although these cells have been known to scientists since the invention of the microscope and have been observed by pathologists in cancerous tissues, their exact function in cancer recurrence remained unknown.
In a recent article in the Journal of Biological Chemistry, an MUSC Hollings Cancer Center research team led by Christina Voelkel-Johnson, Ph.D., reports that it has identified select genes that prostate cancer cells manipulate to become PGCCs, thereby protecting themselves from therapy stress. The Hollings team also found that PGCCs later regain their capacity for cell division, setting the stage for cancer recurrence.
Voelkel-Johnson and her lab made this discovery while studying an inhibitor, or a drug designed to block a biological mechanism, which was associated with durable cures after radiotherapy.
"We initially thought that combination of radiation with the inhibitor killed cancer cells better," said Voelkel-Johnson. "It was only when the inhibitor failed to make a difference in short-term experiments that the time frame was extended, which allowed for an unusual observation."
Lab members had observed giant abnormal-looking cells during the short-term experiments but had considered them to be "doomed." When the time frame was extended, they were surprised to observe that these cells generated small offspring.
"They looked really funky," said Voelkel-Johnson. "When we didn't use the inhibitor, those giant cancer cells generated daughter cells, creating the appearance of a colony with smaller cells surrounding the large one."
These funky-looking PGCCs were visually different from other cancer cells. They were able to make copies of their genetic information, increasing the number of nuclei. However, the cytoplasm was not dividing, and so the cells grew monstrously, containing multiple nuclei instead of only one.
The surprise findings that the monster cells were not "doomed" led Voelkel-Johnson and her team to suspect that their inhibitor stopped cancer recurrence in a different way than they had hypothesized.
"The inhibitor did not kill cancer cells better," said Voelkel-Johnson. "Instead, it prevented the generation of offspring from the polyploid giant cancer cells."
The team also observed that the daughter cells of the PGCCs continued to divide, mimicking tumor recurrence that some patients experience after undergoing therapy. It became clear that this inhibitor was creating durable cures not by causing cell death but by stopping PGCCs from transitioning back into single-nucleus cancer cells with the capacity for division.
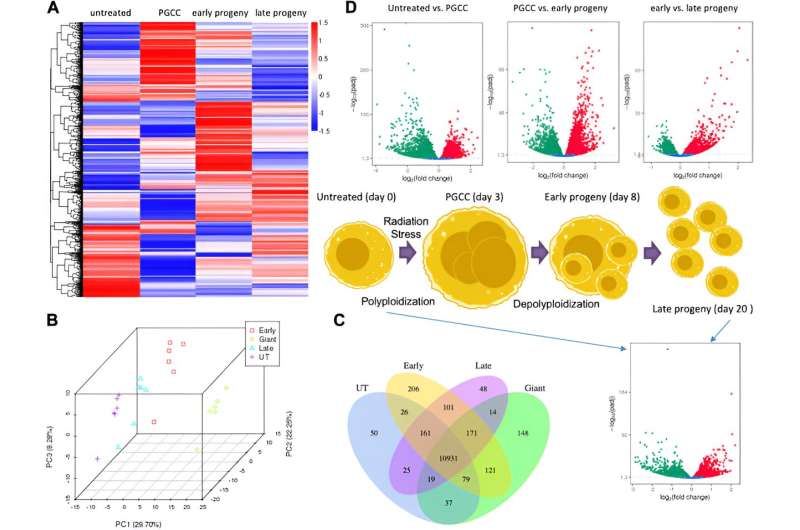
To understand what made PGCCs and their daughter cells different from their parent cancer cells, Voelkel-Johnson, with the help of other collaborators, set out to investigate the changes in gene expression among the different cells that appeared during their experiments. This information would help to explain how cancer cells can transition into and out of PGCC states after being exposed to therapy stress.
Voelkel-Johnson and her team were able to identify cell-signaling pathways that cancer cells manipulate to become PGCCs in response to therapy stress and then later to transition back to cells capable of producing daughter cells.
One protein that specifically piqued their interest was p21, which is induced by a protein called p53 when normal cells are stressed. In normal cells, p21 prevents duplication of damaged DNA, enabling DNA damage to be repaired. Cells in which damage cannot be repaired commit suicide.
The Hollings research team showed that stress in cancer cells lacking p53 also increased p21, but the protein did not stop the duplication of damaged DNA, as it did in normal cells. As a result, p21 helped to set the stage for the generation of the PGCCs.
When increases in p21 were blocked, the stressed cancer cells did not transform into these monstrous cells. Interfering with p21 in cells that were already monstrous prevented them from generating daughter cells that could be responsible for tumor relapse.
The team's findings provide insights into novel mechanisms that could be targeted to improve patient outcomes after cancer therapy. Although it may not be feasible to block p21 as a therapy, both the breast cancer drug tamoxifen and cholesterol-lowering statins have been shown to interfere with the pathways identified by the team. Further research is needed to assess whether they can reduce recurrence rates by blocking PGCCs from regaining the ability to generate daughter cells.
The findings also provide new insight into the optimal timing for the administration of these drugs.
"One of the questions we had was, 'At what point of the therapy do you treat?'" said Voelkel-Johnson. "Our findings suggest that treatment should occur at the same time as chemotherapy or radiotherapy. It is important to administer one of these drugs in conjunction with therapy stress to prevent PGCCs from generating the daughter cell. Once they are generated, it is too late."
Voelkel-Johnson plans to continue to investigate ways to prevent the generation of daughter cells from PGCCs to increase therapy efficacy. She is also interested in assessing how various combination treatment regimens delivered at the time of cancer therapy affect recurrence rates in a wide range of cancers.
More information: Shai White-Gilbertson et al, Transcriptome analysis of polyploid giant cancer cells and their progeny reveals a functional role for p21 in polyploidization and depolyploidization, Journal of Biological Chemistry (2024). DOI: 10.1016/j.jbc.2024.107136




















