Gene therapy method targets tumor blood vessels
Working in mice, researchers at Washington University School of Medicine in St. Louis report developing a gene delivery method long sought in the field of gene therapy: a deactivated virus carrying a gene of interest that can be injected into the bloodstream and make its way to the right cells.
In this early proof-of-concept study, the scientists have shown that they can target tumor blood vessels in mice without affecting healthy tissues.
"Most current gene therapies in humans involve taking cells out of the body, modifying them and putting them back in," said David T. Curiel, MD, PhD, distinguished professor of radiation oncology. "This limits gene therapy to conditions affecting tissues like the blood or bone marrow that can be removed, treated and returned to the patient. Today, even after 30 years of research, we can't inject a viral vector to deliver a gene and have it go to the right place."
But now, investigators at Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine say they have designed a "targetable injectable vector" – a deactivated virus that homes in on the inner lining of tumor blood vessels and does not get stuck in the liver, a problem that has plagued past attempts.
The findings are reported Dec. 23 in PLOS ONE.
Building on their own previous work and others', the researchers engineered this viral vector to turn on its gene payload only in the abnormal blood vessels that help fuel and nurture tumor growth. But unlike most therapies aimed at tumor vasculature, the goal is not to destroy the cancer's blood supply.
"We don't want to kill tumor vessels," said senior author Jeffrey M. Arbeit, MD, professor of urologic surgery and of cell biology and physiology. "We want to hijack them and turn them into factories for producing molecules that alter the tumor microenvironment so that it no longer nurtures the tumor. This could stop the tumor growth itself or cooperate with standard chemotherapy and radiation to make them more effective. One advantage of this strategy is that it could be applied to nearly all of the most common cancers affecting patients."
In theory, Arbeit pointed out, this approach could be applied to diseases other than cancer in which the blood vessels are abnormal, including conditions like Alzheimer's disease, multiple sclerosis or heart failure.
The viral vector Curiel, Arbeit and their colleagues developed contains a section of DNA called ROBO4 known to be switched on in the cells lining blood vessels within tumors.
In mice, the researchers showed that they could inject the vector into the blood stream and that it accumulated in the tumor vasculature, largely avoiding the lung, kidney, heart and other healthy organs.
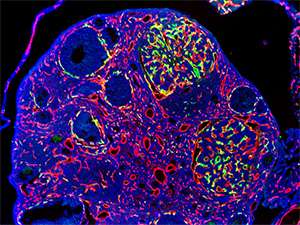
The researchers used the viral vectors to deliver a gene that simply caused cells lining the blood vessels to glow green so they could see whether the vectors gathered in the tumors and bypassed healthy areas.
These mice had tumors in the kidneys and cancerous kidney cells in the skin. In one case, the tumor in the mouse kidney spontaneously spread to an ovary. The investigators showed that the blood vessels feeding the metastatic tumors glowed green but not vessels in the normal part of the ovary.
Adding the anti-clotting drug warfarin also blocked the vector from gathering in the liver by blocking viral interactions with the body's blood-clotting machinery, according to the study. While the researchers say treating cancer patients with warfarin would not be feasible because of the bleeding risk, previous work from their group has shown genetic ways to manipulate the viral vector to prevent it from accumulating in the liver.
"We used a combination of targeting strategies," said Curiel. "We combined a method we had developed to detarget the liver and a method to target the blood vessels. This combination allowed us to inject the vector into the bloodstream of the mouse, where it avoided the liver and found the proliferative vessels of interest to us."
More information: Lu ZH, Kaliberov S, Sohn RE, Kaliberova L, Curiel DT, Arbeit JM. Transcriptional targeting of primary and metastatic tumor neovasculature by an adenoviral type 5 roundabout4 vector in mice. PLOS ONE. Dec. 23, 2013.
















