Immune system memory cells have trick for self preservation
(Medical Xpress) -- After defeating an infection, the immune system creates a memory of the vanquished attacker to make it easier to identify and eliminate in the future. Researchers at Washington University School of Medicine in St. Louis have discovered an important component of the immune system’s strategy for preserving such immunological memories.
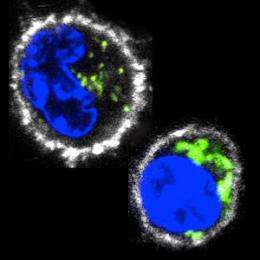
They report online in Immunity that the cells that store these memories, termed memory T cells, enhance their own survival by packing themselves full of energy generators known as mitochondria. The extra mitochondria help the cells live a long time, which in turn extends their ability to help recognize a returning invader. The finding may aid efforts to develop vaccines and to direct the immune system to attack cancers.
Cells typically get most of their energy from glucose and other sugars. When those fuels run low and oxygen is still available, mitochondria allow cells to make energy efficiently from alternative fuel sources such as fats and amino acids.
“These extra mitochondria provide the memory T cells with the flexibility to sustain themselves on a variety of energy sources,” says senior author Erika Pearce, PhD, assistant professor of pathology and immunology. “That significantly boosts their ability to persist in an inactive state for long periods of time and to reactivate if the invader returns.”
T cells have multiple jobs in fighting infection, including recognizing an invader, secreting signals that help mobilize other immune cells and regulating the immune response to minimize collateral damage to the body. To do these jobs, they differentiate into various specialized T cell types, such as the memory T cell.
In earlier research, Pearce showed that when memory T cells develop as a result of an infection, they change the way they generate energy. Her data suggested that mitochondria likely play an important part in this metabolic switch.
For the new study, Rianne van der Windt, PhD, a postdoctoral researcher in the lab, gave a drug that forces mitochondria to work at maximum capacity to T cells that had never encountered a pathogen, T cells that specialized in actively fighting infection and memory T cells. She monitored the cells’ consumption of oxygen, an indicator of how much they are using their mitochondria to make energy.
Memory T cells were the only T cells to significantly increase their consumption of oxygen after exposure to the drug, suggesting that they somehow maintained a considerable reserve energy-generating capacity in their mitochondria that the other T cells lacked.
When van der Windt measured numbers of mitochondria in the T cells, she found that memory T cells had many more mitochondria. She hypothesized that the extra energy generating capacity that comes with more mitochondria allows memory T cells to live for long periods of time and to power-up again if an invader is re-encountered.
“In follow-up experiments, we showed that production of additional mitochondria is triggered by interleukin-15, an immune signaling factor long known to be important to memory T cells,” says Pearce. “We also found that by genetically manipulating T cell’s mitochondria and causing them to switch to the energy-making methods favored by the memory cells, we could cause a higher percentage of undifferentiated T cells to become memory cells.”
Pearce notes that T cells that lack extra mitochondria can rapidly proliferate when the immune system is fighting an infection, but they die off almost as rapidly when the infection is cleared. She thinks that further consideration of what makes T cells stable could be helpful to researchers working to use T cells to attack tumors.
These projects typically involve removing the patient’s T cells, training them to recognize the tumor and exposing them to an immune signaling factor that makes the cells proliferate. The cells are then injected back into the patient.
“If these cells are pushed too hard and don’t see the signals that normally accompany an immune reaction, they’re all going to die fairly quickly,” Pearce says. “To produce a lasting and effective immune response, I think we need to pay more attention to what the mitochondria look like in T cells.”
It may be possible to use interleukin-15 and other agents that promote creation of mitochondria to help these cells persist longer, according to Pearce.
Further studies of how mitochondria are organized in memory T cells are underway in Pearce’s laboratory. She is also collaborating with vaccine researchers to see if new insights into memory cells can aid the development of preventive treatments for pathogens that have proven difficult to vaccinate against, such as HIV and Leishmania.
More information: van der Windt GJW, Everts B, Chang C-H, Curtis JD, Freitas TC, Amiel E, Pearce EJ, Pearce EL. Mitochondrial respiratory capacity is a critical regulator of CD8+ T cell memory development. Immunity, online 12/29/11.














