Grant to fuel baking soda cancer therapy research

A $2 million grant from the National Institutes of Health will enable University of Arizona biomedical engineering researchers to improve the way doctors measure the effectiveness of drinking baking soda to fight breast cancer.
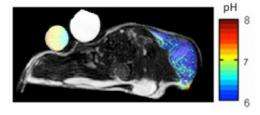
The grant will be used to help refine a new magnetic resonance imaging method for measuring pH, or acid content, of a tumor that has been discovered in a patient but not yet treated.
By measuring the acid content of the tumor, doctors can monitor the effectiveness of personalized treatments such as baking soda on both tumors and healthy tissue, and even predict the effectiveness of chemotherapies before the patient starts the medication.
Drinking baking soda has been proven to reduce or eliminate the spread of breast cancer to the lungs, brain and bone, but too much baking soda can also damage normal organs.
"In other words, this test is designed to lead to personalized medicine for cancer patients, by optimizing the therapy to each individual," said Mark "Marty" Pagel, UA associate professor of biomedical engineering and lead researcher on the project.
Just as people feel the burn from lactic acid produced in their muscles during rigorous exercise, tumors also produce lactic acid when they are actively growing, Pagel said. This acid destroys surrounding tissue, which allows the tumor to grow, invade surrounding areas, and metastasize to other organs in the body. "The acid also provides resistance to common chemotherapies," Pagel said.
"Measuring the pH in a tumor is essential, because some drugs only work at the right pH," said Jennifer Barton, professor and head of UA biomedical engineering. "Patients can actually change their body's pH to make their cancer drugs more effective – it can be as simple as drinking baking soda – but this process has to be carefully monitored."
The goal of the research is to prove that this unique and innovative MRI tumor measurement technique will help improve, and in some cases save, the lives of women with breast cancer.
The study is being conducted in collaboration with Dr. Ian Robey, assistant professor of research at The University of Arizona Cancer Center, and clinical collaborators Drs. Alison Stopeck, Setsuko Chambers and Phil Kuo, who are refining the new methodology to give doctors the ability to directly diagnose the acid content in tumors of cancer patients.
"This is a tool that is currently available to very few scientists across America," Pagel said. "So we have recently collaborated with the Barrow Neurological Institute and other sites in Phoenix to implement our methods in their research centers. These collaborations demonstrate that this method can assist in the individual, personal treatment of breast cancer patients around the world."
Pagel said another unique aspect of this research is the discovery that a chemical agent already approved for clinical X-ray imaging can also be used for MRI studies, allowing clinical trials to begin without approval from the U.S. Food and Drug Administration.
Pagel cited a generous gift from the Community Foundation of Southern Arizona as support for the initial development of the new method, and a recent gift from the Phoenix Friends of the Arizona Cancer Center that has let researchers begin the process of bringing the method to the cancer clinic level.
"These gifts supported the critical innovations in our research that led to the $2 million grant from the National Institutes of Health," he said. "This demonstrates the tremendous value of private support for innovative research at the University of Arizona."












