Problems in recycling cellular waste linked to clogged arteries
(Medical Xpress) -- Researchers at Washington University School of Medicine in St. Louis have found that problems with a digestive process in cells can clog arteries.
The finding could provide a target for future therapies aimed at preventing or reversing atherosclerosis, a common disorder in which fat, cholesterol and other substances build up in the walls of arteries and block blood flow.
The study found that disruptions in cell digestion, called autophagy, caused drastic inflammation in artery walls, a common characteristic of atherosclerosis.
The researchers report the finding in the April 4 issue of the journal Cell Metabolism.
“Good digestion in the cell allows it to recycle garbage,” says first author Babak Razani, MD, PhD, an instructor in medicine. “If too much protein builds up or parts of the cell become dysfunctional, this digestive process recycles and reuses parts of cells and discards parts that aren’t working properly.”
The researchers note that ancient Egyptian physicians believed vascular disease was the result of an accumulation of undigested food in blood vessels. The new findings suggest that those ancient scholars were partly right.
“People have developed atherosclerosis for thousands of years, even before they ate fast food or worked at sedentary jobs,” says senior investigator Clay F. Semenkovich, MD. “The ancient hypothesis about chronic diseases said that many problems came from undigested food, and from our experiments, it looks like there is, in fact, a good deal of undigested cellular food that collects in atherosclerotic lesions.”
Razani and Semenkovich, the Herbert S. Gasser Professor of Medicine, professor of cell biology and physiology and director of the Division of Endocrinology, Metabolism and Lipid Research, worked with Herbert W. Virgin IV, MD, PhD, the Edward Mallinckrodt Professor and head of the Department of Pathology and Immunology and professor of molecular microbiology and of medicine. The interdisciplinary team studied mice with high cholesterol that develop atherosclerosis. They found that as plaques formed in the blood vessels and the atherosclerosis got worse, the mice were also having problems with cellular digestion.
“This recycling process keeps cells healthy, and a number of disease states have been linked to dysfunction in that process,” Razani says. “Atherosclerosis involves cellular dysfunction, so you could imagine that cellular recycling might be important, but no one had tested the idea.”
Atherosclerosis is common in the U.S. and throughout the Western world, and heart disease linked to atherosclerosis is the leading cause of heart attack and stroke in Western countries. Nearly 800,000 heart attacks and a similar number of strokes occur each year in the U.S., causing more than one in every five deaths.
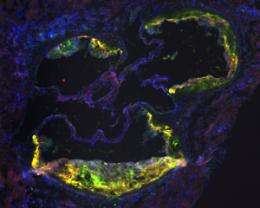
Razani says another key component of atherosclerosis is chronic inflammation in the walls of arteries, caused mainly by the accumulation of white blood cells called macrophages. And it’s in those macrophages where autophagy breaks down.
“When we disrupted the recycling of cellular waste in macrophages, the animals had much more atherosclerosis,” he says. “And the reason was that these mice had a lot more inflammation.”
Earlier studies had speculated that disrupting cellular digestion and recycling might lead to more inflammation, and in this study the researchers showed that when the cellular digestion mechanism was impaired, mice released very large amounts a key inflammatory marker called interleukin 1-beta (IL-1ß).
“When recycling was disrupted in macrophage cells, IL-1ß went through the roof,” Razani says. “We discovered that the mechanism generating that IL-1ß was a collection of proteins called an inflammasome, which is, essentially, several proteins that come together to tell the system to secrete inflammatory substances such as IL-1ß. When there is a problem with recycling of cellular waste, these inflammatory proteins go into hyper-drive.”
The more of the inflammatory substance secreted, the higher the levels of inflammation and worsened atherosclerosis. The new study suggests that vicious cycle centers on cellular digestion and recycling. The next step will involve searching for ways to ramp up the cellular digestion process. The researchers already have identified strategies that might be useful.
“One is fasting,” Semenkovich says. “In the fasting state, cells use this mechanism to recycle proteins and discard garbage. Increased autophagy may be why a low-calorie diet reduces atherosclerosis and heart attacks.”
A drug used to prevent organ rejection in transplant patients also might point the way to more effective therapies. Previous studies have found that the drug, called rapamycin, can reduce atherosclerosis in mice. The researchers are planning to test rapamycin in mice to see whether it induces cell recycling in animals with atherosclerosis.
The problem is that rapamycin has a lot of side effects, Semenkovich says. It may decrease atherosclerosis, but lipids get much worse, so people are very nervous about giving the drug to patients who already have cholesterol problems. However, if it were possible to deliver rapamycin, or a similar substance, to specific areas where plaques are located, that might be a potential strategy for treatment.
“It’s probably not the best drug to use in people, but if we can demonstrate that it is indeed reducing atherosclerosis by revving up cell digestion and recycling, then we’d have a proof of principle,” Razani says. “From there, we might be able to look for ways to deliver the drug directly to plaques or perhaps find other drugs that improve autophagy and may help prevent or delay some of the catastrophic problems associated with atherosclerosis.”
More information: Razani B, Feng C, et al, Autophagy links inflammasomes to atherosclerotic progression. Cell Metabolism, vol. 15(4), April 4, 2012.

















