Ills of aging blood: Short-circuited stem cell programming linked to failing blood development
As blood stem cells age, changes in the epigenome—the system that regulates which genes are switched on and which are switched off throughout the body—alter these cells in ways that lead to reduced immune response, increased anemia and rising risk of certain leukemias, researchers have found.
The findings were published online in Cell Stem Cell on Feb. 14, 2013.
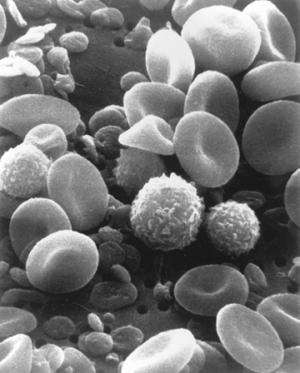
Hematopoetic stem cells, or HSCs, contain the basic blueprint for all blood cells, and so can create and renew the body's supply of red blood cells, immune cells and all of the other diverse cell types in the blood system. In older individuals—a two-year-old mouse or an 80-year-old human—the blood-building system begins to falter: fewer T and B cells leads to lowered immune response, and fewer red blood cells leads to anemia. What's more, the risk of blood cancers rises.
Since these changes all arise from the system that creates new blood cells, researchers at Harvard Medical School and Harvard University wanted to see if there was a common failing in the epigenome of HSCs that cascaded down the hierarchy of progenitor cells, causing the distinct failings of diverse blood cells.
On-off switches for genes
The epigenome is a kind of control system for the genome, a system of molecules that attach to, and surround, DNA. Through their physical and chemical interactions with the genome, these molecules help determine which genes are turned on and off in different stages of life and in different kinds of cells. They help define the difference between fetal development and puberty, or between a red blood cell and a platelet. If the genome is a circuit, the epigenome contains the switches, dials and resistors that can modulate the flow of current.
"What we discovered is that as an individual ages, the epigenome is modulated in stem cells a very specific manner that clearly impacts the function of these cells by changing their ability to produce certain types of blood cells," said Derrick Rossi, assistant professor of stem cell and regenerative biology at Harvard University, HMS assistant professor of pathology and investigator in the Program in Cellular and Molecular Medicine at Boston Children's Hospital, and a senior author of the study.
While the researchers found that the epigenome of HSCs is very stable overall, they noted specific changes in sites that clearly influence the ability of the stem cells to form particular kinds of blood cells. This loss of cell production capacity correlates with specific ways that the blood system declines in aging.
The epigenetic changes observed in the study mostly targeted genes that are crucial for the development of downstream blood cells but are not expressed in HSCs themselves. The data further suggest that these epigenomic changes manifest their impact on blood cell production by diminishing the stem cells' ability to give rise to immune cells, and also by increasing the production of cell types typically involved in myeloid diseases associated with aging.
"These findings highlight the additional power gained through epigenomic analysis and strengthens our mechanistic understanding of the aging process," said Alex Meissner, associate professor of stem cell and regenerative biology at Harvard University, a senior author of the study.
Tracking rare cells
To study the epigenetic changes in aging HSCs, the researchers analyzed samples of these cells from young and old mice using a high-throughput, deep epigenome sequencing technique developed in Meissner's lab. They also measured the functional capability of the different samples of cells by transplanting them into irradiated mice lacking all blood cells, to see how well they could replace the animal's supply of blood cells. Some cell samples were subjected additional stress by being forced to multiply from low transplant levels and other challenges.
When researchers identified changes in the epigenome, they determined through genetic analysis which genes were affected.
The particular epigenetic marker that the researchers studied is called DNA methylation, in which a methyl group is added to one of the nucleotide building blocks of DNA. Such modifications can lead to changes in gene expression and protein production. This DNA tagging is generally a permanent mark akin to twisting off a wire pair and capping it in a circuit. It is a durable, heritable change that can be passed from a cell to all of its daughter cells.
Another component of the epigenome, histones, are involved in packaging the DNA and upon modification make certain genes more or less accessible to being expressed. In general, histone modifications are more dynamic than DNA methylation, and can also be used to modulate genes. Histones can twist tightly or loosely around genes, turning their expression down or up like a volume knob controls the level of sound on a stereo.
Histone modifications are near impossible to study directly in rare cell types like HSCs. HSCs make up only about 1 in 20,000 cells in the bone marrow, which means each mouse only has around 2,000 of these cells. To analyze a histone profile, millions of cells are needed. However, with DNA methylation, Meissner's high-throughput platform allowed the researchers to amplify the samples in a way that preserves the DNA methylation tags so that a few hundred cells can produce enough material to analyze on a global scale.
Shorting out the circuit
Strikingly, the researchers' analysis showed that genes targeted by DNA methylation during HSC aging were associated with a different kind of epigenetic regulator called polycomb repressive complex 2 (PRC2), which acts by modifying histones to form a kind of switch that is turned off in HSC, but can be flipped on in the intermediary cells that form specific blood cells.
The more permanent DNA methyl tags appear to be taking the place of PRC2 regulated histones, turning a quick-flick switch into a dead circuit. The authors also show that the core components of PRC2 decline in the HSCs with age. The fact that PRC2 loss is implicated in the wide array of aging-related changes and diseases in the blood system suggests that PRC2 is an important element in the process of aging in blood.
But unlike genetic changes, even these more durable epigenetic changes remain adaptable. "In contrast to genetic damage such as DNA mutations which is permanent, the epigenome is much more malleable," Rossi said, noting that in myelodysplastic syndrome, one of the canonical diseases of aging in the blood system, many cases are known to be responsive to hypomethylating agents, which remove DNA methyl tags, bringing switched-off genes back on-line and allowing damaged cells to heal and renew themselves properly.
"Understanding the underlying biology in the blood stem cells during aging will be crucial not only for deepening our fundamental understanding of the science of aging, but also for understanding the evolution of disease and providing insights that may be harnessed therapeutically," Rossi said.
















