Brain processes ongoing pain more emotionally
A momentary lapse of concentration is all it takes for a finger to become trapped or sprain an ankle - and it hurts. Pain is the body's protective mechanism and a complex neurological phenomenon. Moreover, ongoing pain in the sense of chronic pain can be a disease. Scientists from Technische Universität München (TUM) have now demonstrated that already during a few minutes of ongoing pain, the underlying brain activity changes by shifting from sensory to emotional processes.
In their experiments, Prof. Markus Ploner, Heisenberg Professor for Human Pain Research at the TUM School of Medicine, and his team investigated pain perception: How does the duration of pain or the action of a placebo affect activities in the brain? For their measurements they used electroencephalograms (EEGs). The test subject wore a cap with 64 electrodes that can measure nerve cell activity in the brain throughout the experiment. This method makes it possible to chronologically pinpoint which signals nerve cells use to respond to a pain stimulus.
Pain influences emotion
The scientists used the following arrangement for their experiments: Over a period of ten minutes, 41 participants in the study were given painful heat stimuli to the hand which varied in intensity throughout the duration of the experiment. The participants were asked to continuously assess the level of their pain on a scale of one to a hundred with the other hand using a slider.
"We were absolutely amazed by the results: After just a few minutes, the subjective perception of pain changed - for example, the subjects felt changes in pain when the objective stimulus remained unchanged. The sensation of pain became detached from the objective stimulus after just a few minutes," says Markus Ploner, describing the results.
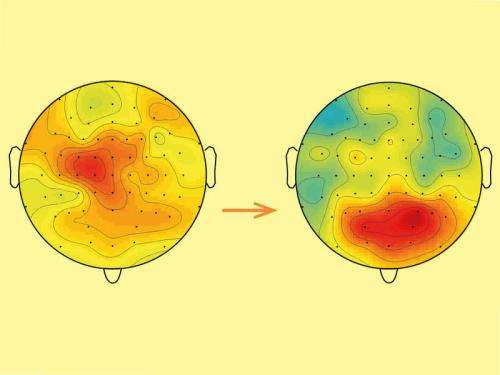
Previous studies showed that brief pain stimuli are predominantly processed by sensory areas of the brain that process the signals from the sensory organs such as the skin. However, in their experiment with longer-lasting ongoing pain, the EEGs gave the scientists a different picture: in this case, emotional areas of the brain became active.
"If pain persists over a prolonged period of time, the associated brain activity shows that it changes from a pure perception process to a more emotional process. This realization is extremely interesting for the diagnosis and treatment of chronic pain where pain persists for months and years," explains Markus Ploner, who is also senior physician in the Department of Neurology at the TUM Klinikum rechts der Isar.
Placebos change the perception of pain
A second experiment showed that it is not just the duration, but also the anticipation of a pain stimulus that affects perception. Twenty test subjects were initially given different intensities of painful laser pulses on two areas of the back of the hand. The participants then rated verbally how strong they perceived the pain stimuli. As the experiments progressed, the subjects were once again given the same stimuli, the difference this time being that two creams had previously been applied to both areas. Although neither cream contained an active substance, the subjects were told that one of the creams had a pain-relieving effect.
The result according to Markus Ploner: "The subjects assessed the pain on the skin area with the allegedly pain-relieving cream as significantly lower than on the other area of skin." The scientists were further able to demonstrate how the brain implements this placebo effect: although the subjects were given the same pain stimuli, the nerve cells in the second run triggered a different pattern of brain activity.
"Our results show how differently our brain processes the same pain stimuli. Systematically mapping and better understanding this complex neurological phenomenon of 'pain' in the brain is a big challenge, but is absolutely essential for improving therapeutic options for pain patients," in Ploner's opinion.
More information: E. Schulz, E. S. May, M. Postorino, L. Tiemann, M. M. Nickel, V. Witkovsky, P. Schmidt, J. Gross, M. Ploner, Prefrontal gamma oscillations encode tonic pain in humans, Cerebral Cortex, February 2015. DOI: 10.1093/cercor/bhv043
L. Tiemann, E. S. May, M. Postorino, E. Schulz, M. M. Nickel, U. Bingel, M. Ploner, Differential neurophysiological correlates of bottom-up and top-down modulations of pain, Pain, 2015, Feb;156(2):289-96. DOI: 10.1097/01.j.pain.0000460309.94442.44



















