Researchers develop new strategy to limit side effects of stem cell transplants
Scientists in Germany have developed a new approach that may prevent leukemia and lymphoma patients from developing graft-versus-host disease (GvHD) after therapeutic bone marrow transplants. The researchers describe the successful application of their strategy in mice in "Exogenous TNFR2 activation protects from acute GvHD via host T reg cell expansion," which will be published online August 15 ahead of issue in The Journal of Experimental Medicine.
Bone marrow transplants can cure types of leukemia and lymphoma because hematopoietic stem cells derived from the donor's bone marrow can develop into immune cells capable of killing the patient's tumor cells. But the donor-derived immune cells may also attack the transplant recipient's healthy tissues, producing the diverse and sometimes severe symptoms of GvHD. One approach to avoiding GvHD is to co-transplant large numbers of regulatory T cells (T reg cells), immune cells that can suppress the donor cells' effects on healthy tissue while maintaining their ability to kill tumor cells. This approach is challenging, however, because the T reg cells must first be isolated from the donor's peripheral blood or bone marrow and then cultivated in the laboratory to produce sufficient numbers for transplantation.
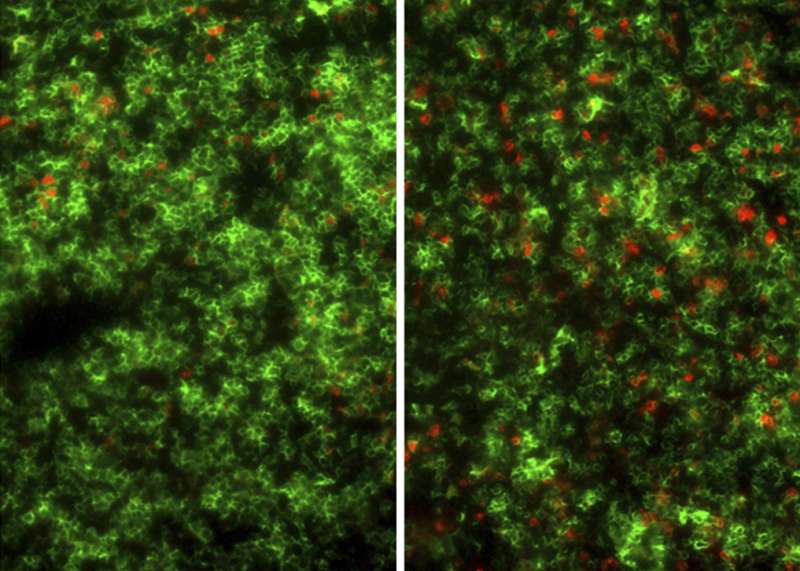
A team of researchers led by Andreas Beilhack and Harald Wajant of the University Hospital W?rzburg devised an alternative way to prevent GvHD in mice, developing a protein called STAR2 that can stimulate the formation of the transplant recipient's own T reg cells in vivo. Pretreating mice with STAR2 protected them from developing GvHD after immune cell transplantation. The donor-derived cells retained their ability to kill the recipient's lymphoma cells, however.
STAR2 works by specifically binding to a cell surface protein called TNFR2, activating a signaling pathway that increases the number of T reg cells. Beilhack and colleagues found that a slightly modified version of STAR2 has a similar effect on human T reg cells, suggesting that the approach could also prevent GvHD in leukemia and lymphoma patients after bone marrow or hematopoietic stem cell transplants. "Furthermore, this strategy may be beneficial for other pathological settings in which elevated numbers of regulatory T cells are desirable, such as autoimmune diseases and solid organ transplantation," Beilhack says.
More information: Chopra, M., et al. 2016. J. Exp. Med. DOI: 10.1084/jem.20151563
















