Structure of toxic tau aggregates determines type of dementia, rate of progression
The distinct structures of toxic protein aggregates that form in degenerating brains determine which type of dementia will occur, which regions of brain will be affected, and how quickly the disease will spread, according to a study from the Peter O'Donnell Jr. Brain Institute.
The research helps explain the diversity of dementias linked to tau protein aggregation, which destroys brain cells of patients with Alzheimer's and other neurodegenerative syndromes. The study also has implications for earlier and more accurate diagnoses of various dementias through definition of the unique forms of tau associated with each.
"In addition to providing a framework to understand why patients develop different types of neurodegeneration, this work has promise for the development of drugs to treat specific neurodegenerative diseases, and for how to accurately diagnose them. The findings indicate that a one-size-fits-all strategy for therapy may not work, and that we have to approach clinical trials and drug development with an awareness of which forms of tau we are targeting," said study author Dr. Marc Diamond, founding Director of the Center for Alzheimer's and Neurodegenerative Diseases, and Professor of Neurology and Neurotherapeutics with the O'Donnell Brain Institute at UT Southwestern Medical Center.
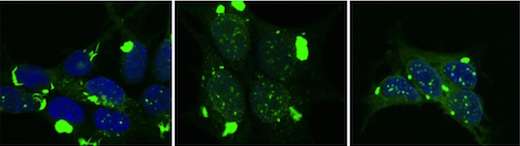
Researchers used special cell systems to replicate distinct tau aggregate conformations. These different forms of pathological tau were then inoculated into the brains of mice. Each form created different pathological patterns, recapitulating the variation that occurs in diseases such as Alzheimer's, frontotemporal dementias, and traumatic encephalopathy.
The different forms of tau caused pathology that spread at different rates through the brain, and affected specific brain regions. This experiment demonstrated that the structure of pathological tau aggregates alone is sufficient to account for most if not all the variation seen in human neurodegenerative diseases that are linked to this protein.
The finding, published in Neuron, could have a notable impact on widespread efforts at the O'Donnell Brain Institute and elsewhere to develop treatments that eliminate tau and other toxic proteins from the brains of dementia patients.

"The challenge for us now is to figure out how to rapidly and efficiently determine the forms of tau that are present in individual patients, and simultaneously, to develop specific therapies. This work says that it should be possible to predict patterns of disease in patients and responses to therapy based on knowledge of tau aggregate structure," said Dr. Diamond, who holds the Distinguished Chair in Basic Brain Injury and Repair.
Dr. Diamond's lab, at the forefront of many notable findings relating to tau, had previously determined that tau acts like a prion - an infectious protein that can self-replicate and spread like a virus through the brain. The lab has determined that tau protein in human brain can form many distinct strains, or self-replicating structures, and developed methods to reproduce them in the laboratory. This research led Dr. Diamond's team to the latest study to test whether these strains might account for different forms of dementia.
To make this link, 18 distinct tau aggregate strains were replicated in the lab from human neurodegenerative disease brain samples, or were created from mouse models or other artificial sources. Researchers inoculated the strains into different brain regions of mice and found striking differences among them.
While some strains had far reaching and rapid effects, others replicated only in limited parts of the brain, or caused widespread disease but did so very slowly. This surprising result answered a fundamental question that has dogged the field of neurodegenerative disease: Why are brain regions vulnerable in certain cases but not others, and why do some diseases progress more rapidly than others?
For instance, in Alzheimer's disease, problems begin in brain memory centers before spreading to other areas that control functions such as language. Conversely, due to initial degeneration of frontal and temporal brain regions in frontotemporal dementia, the memory centers are relatively spared, and patients often first show changes in personality and behavior.
The new study implies that with knowledge of tau aggregate structure in patients, or possibly even in healthy individuals, it should be possible to predict the brain regions most vulnerable to degeneration and the rate of disease progression.
More information: Sarah K. Kaufman et al. Tau Prion Strains Dictate Patterns of Cell Pathology, Progression Rate, and Regional Vulnerability In Vivo, Neuron (2016). DOI: 10.1016/j.neuron.2016.09.055



















