How killer cells take out tumors
The use of immunotherapy to treat cancer is celebrating its first successes – but there are still many knowledge gaps in the underlying mechanisms of action. In a study of mice with soft tissue tumors, ETH researchers have now shown how endogenous killer cells track down the tumors with the help of dormant viruses.
The promising drug is known as F8-TNF. When injected into the bloodstream, it lures killer cells from the body's immune system towards sarcomas. The killer cells then destroy the tumors. Researchers from ETH Zurich, led by Professor Dario Neri at the Institute of Pharmaceutical Sciences, developed F8-TNF four years ago. Since then, they have been able to show that it can completely cure sarcomas in mice when combined with a chemotherapeutic agent. Such an effective treatment cannot be achieved by chemotherapy alone or with other therapeutic approaches. Now, a drug closely related to F8-TNF is being tested as part of clinical trials in humans.
Consisting of two sub-units, the F8-TNF molecule works rather like a store detective: just as a detective tracks down a shoplifter and detains it until the police arrive, the molecule identifies cancer cells using its F8 sub-unit and then uses its TNF part to lure killer cells (cytotoxic T cells). TNF is an immune system messenger.
Implanted into the genome
Much of the molecule's mechanism of action was hitherto unclear, but the scientists in Neri's group have now succeeded in working it out. They wanted to find out how the killer cells recognize the tumor after they are lured to it. Although the messenger TNF alerts the killer cells to the tumor's presence, it does not provide them with a specific tumor identifier.
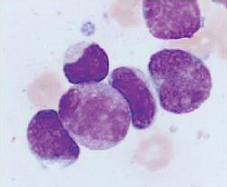
The scientists discovered that the killer cells called by F8-TNF are guided by proteins from specific dormant viruses (endogenous retroviruses). The genetic blueprint of these viruses has implanted itself into the mouse genome during evolution. In many cancer cells, the viral proteins are brought to life. Fragments of these retroviral proteins on the surface of tumor cells allow the killer cells to distinguish cancer cells from healthy cells.
Immune protection against cancer
In addition, the scientists observed that mice where the sarcomas were cured with F8-TNF rejected tissue later transplanted from various types of tumor. "The mice appeared to have acquired a sort of immune protection against cancer. As it turned out, this protection is also due to the killer cells, which recognize the tumor cells with the help of dormant viral proteins," says Philipp Probst, a doctoral student in Neri's group.
In cancer immunotherapy, the body's immune system is activated in order to combat tumors. In the past, many scientists assumed that the killer cells used modified proteins on the surface of tumor cells as an identifier and a point of attack. Tumors are a degenerate form of body tissue; they are formed as a result of certain genetic mutations in a precursor cell, which can lead to protein modifications. "In some cases, mutated proteins can indeed be the distinguishing criterion," says Neri. "In our paper, however, we confirm that killer cells can also use other distinguishing criteria, namely the presence or absence of retroviral proteins."
Aid to understanding
"Now we cannot only cure sarcomas in mice, but also know the mechanism behind this therapy," says Probst. In the relatively new field of cancer immunotherapy, it is important to understand the underlying mechanisms in order to predict which patients will respond best to which therapy.
Further research will be needed to find out whether the observations in mice also apply to humans, as the human genome is full of gene sequences from dormant viruses. In any case, the knowledge may be useful in the interpretation of clinical trials. The third and final phase clinical trials in humans for the active agent L19-TNF, which is related to F8-TNF, will soon begin in Germany; in the US, applications for such trials are currently being examined by the authorities.
Cancer immunotherapy 100 years ago
More than 100 years ago, New York-based doctor William Coley had already observed that some sarcoma patients recovered spontaneously. These were all patients suffering not only from cancer but also from a bacterial infection. Coley attempted to convert his observation into a therapeutic approach and began to inject sarcoma patients with a cocktail of heat-inactivated bacteria. His experiments were successful and "Coley's toxin" became the therapy of choice for sarcoma patients in the early decades of the 20th century. Although it was later displaced to some extent by radiotherapy and the emerging field of chemotherapy, "Coley's toxin" was still manufactured in Germany until 1990.
In Coley's time, knowledge was not yet advanced enough to understand his cocktail's mechanism of action. From today's perspective, one must assume that the inactivated bacteria triggered an immune response and thus the formation of the messenger TNF. In turn, this messenger activated killer cells that fought the tumor.
More information: Philipp Probst et al. Sarcoma eradication by doxorubicin and targeted TNF relies upon CD8+ T cell recognition of a retroviral antigen, Cancer Research (2017). DOI: 10.1158/0008-5472.can-16-2946
















