Checkpoint inhibitors fire up different types of T cells to attack tumors
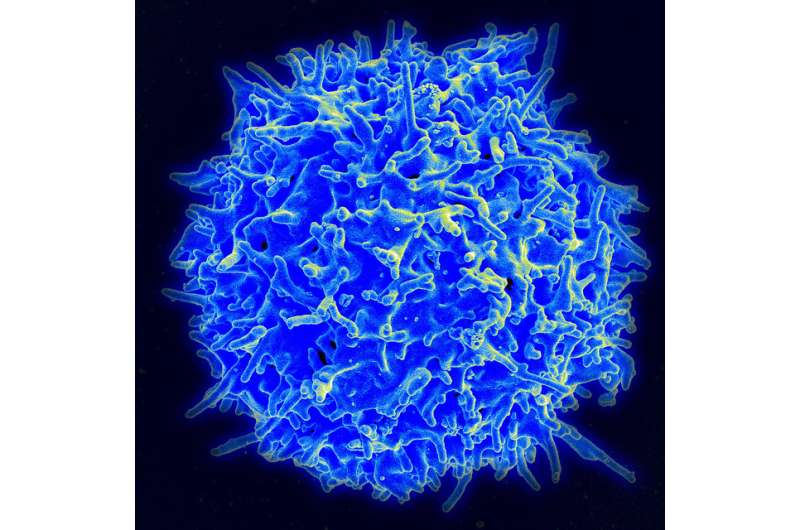
Cancer immunotherapies that block two different checkpoints on T cells launch immune attacks on cancer by expanding distinct types of T cell that infiltrate tumors, researchers from The University of Texas MD Anderson Cancer Center report in the journal Cell.
"The mechanisms these two therapies use mostly do not overlap, which provides a reason why combining them works better than either alone," said Jim Allison, Ph.D., chair and professor of Immunology at MD Anderson.
Researchers analyzed infiltrating immune cells from mouse tumor models and human melanomas treated with either anti-CTLA-4 or anti PD-1 checkpoint inhibitors. Using mass cytometry, they analyzed 33 surface markers and 10 intracellular markers to characterize infiltrating cells.
"The clinical successes of checkpoint blockade have gotten out ahead of our understanding of how these drugs work," Allison said. "In some ways, that's a good problem to have, but we need greater understanding of the basic science behind these drugs to use them more effectively for patients."
Uncovering the cellular mechanisms used by each type of checkpoint inhibitor opens the door to more precise understanding of how to use the drugs separately and in combination with each other and other types of therapy, Allison said.
When they analyzed immune infiltrates, lead author Spencer Wei, Ph.D., a postdoctoral fellow in Allison's lab, and colleagues found:
- Anti-CTLA-4 treatment expands the presence of CD4 effector T cells that are positive for ICOS, an immune-stimulating protein, and that these cells were strongly associated with smaller tumors in the mice.
- Anti-PD-1 and anti-CTLA-4 treatment greatly expands the presence of CD8 T cells, the most powerful killers in the T cell family, and they were associated with smaller tumors in the mice.
- These PD-1 positive CD8 T cells had what scientists call an exhausted-like phenotype. They have markers of inactivity, including the presence of other immune checkpoints, but are not necessarily known to be inactive and likely still have significant functional activity.
"These cells are boosted by anti-PD-1, but they keep their exhausted phenotype, which suggests they'll shut down when the PD-1 antibody is withdrawn," Allison said. This supports the need to give the drug for long periods, and current anti-PD-1 regimens provide a year or two of treatment.
The team ran these experiments in a mouse model of melanoma known to be highly immunogenic, so vulnerable to immunotherapy, and one model that is poorly immunogenic - "more like prostate cancer than melanoma," Allison said.
The two drugs worked by expanding the same T cell infiltrates in both tumor types, so their mechanisms appear to be independent of tumor characteristics, but tumor characteristics are likely to affect the magnitude of responses.
Subsequent analyses of surgically removed human melanoma tumors showed that anti-CTLA-4 and anti-PD-1 each expanded T cell populations analogous to those found in the mouse models.
Additional research is needed to confirm and further understand these findings in larger studies, the researchers note.
Allison invented immune checkpoint blockade as a cancer therapy with his research leading to development of ipilimumab (Yervoy), and an approach of treating the immune system, rather than the tumor directly. By blocking CTLA-4, a protein on T cells that shuts down immune responses, ipilimumab unleashed the adaptive immune system to attack cancer.
Subsequently, other researchers developed inhibitors that block PD-1, a separate brake on T cells, or its main activating ligand, PD-L1, found on tumors and on normal cells.
Ipilimumab has been approved by the U.S. Food and Drug Administration alone or in combination against metastatic or inoperable melanoma. Two PD-1 inhibitors have been approved for melanoma, lung, bladder, kidney, head and neck cancers and non-Hodgkin lymphoma. Several PD-L1 inhibitors have also been approved for use in multiple tumor types.
CTLA-4 blockade is thought to act at the initiation of immune response, while PD1 is used by tumors to shut down an immune response that is under way by using PD-L1 to turn T cells off. About 15 to 25 percent of patients respond to these drugs, and researchers are seeking biomarkers to guide treatment and exploring new combinations to improve and expand responses.

















