When the nose doesn't know: Can loss of smell be repaired?
Researchers at Tufts University School of Medicine, led by Dr. James E. Schwob, are examining the behavior of adult stem cells within the context of aging and, specifically, the sense of smell. As part of the normal aging process, older adults frequently experience a decline in their olfactory function, resulting in a compromised or complete loss of sense of smell. The loss of sense of smell—whether as a result of aging, medication, illness or injury—affects sense of taste; when the sense of smell is intact, it combines with the sense of taste to communicate the flavor of food. Smell loss in older adults reduces quality of life, compromises nutritional status, and puts the health and safety of the elderly at risk.
The focus of the research at Tufts is on enlarging the population of adult stem cells that maintain the sense of smell in young adults, but which deteriorate with aging. The ultimate goal is to identify a pharmaceutical preparation that has that effect.
In a study published in the December 7 issue of Cell Stem Cell, the researchers provide the first evidence that it is possible to regenerate stem cells of the nasal tissue in mice, thus enlarging the population of adult stem cells.
Stem cells are undifferentiated, or unspecialized; they are highly potent and able to generate many different types of cells. Embryonic stem cells can give rise to any cell type in the body, while adult or tissue stem cells have a more limited potency. Adult stem cells are responsible for maintaining the structure of the tissue in which they are found and repairing it after injury. There is evidence that adult stem cells may be able to regenerate in response to injury to tissue as part of a natural healing process.
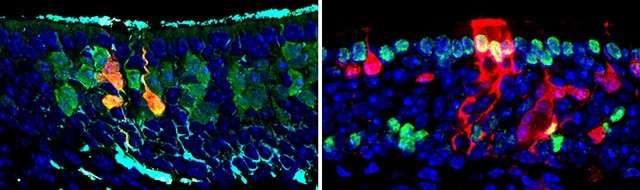
The team took advantage of that natural healing process. Adult stem cells regenerated in mice with injured nasal tissue. When those adult stem cells were transplanted into other mice, they were able to regenerate all the different cell types in the nasal tissue, also called the olfactory epithelium. This expansion of the stem cell population improved when the researchers swabbed a pharmaceutical preparation into the nose; the drug combination pushed progenitor cells to remain upstream as adult stem cells.
Though the response involved the now-famous Yamanaka factors, the strategy developed by Schwob and his team is more efficient and less complicated than the induced pluripotent stem cell (iPSC) Nobel Prize-winning approach developed by Dr. Shinya Yamanaka. Yamanaka's approach was designed to replace stem cells lost to aging by inducing cells taken from adult tissues to behave like embryonic stem cells, by forcing them to express four genes that are usually expressed in embryonic stem cells.
The research team from Tufts determined that only two of the four factors used by Yamanaka to artificially reprogram adult cells into iPSCs are critical to the process of pushing the olfactory cells to become more stem cell-like.
"We are the first researchers to gain insight into the molecular mechanism responsible for allowing these adult progenitor cells to become more potent. We were intrigued that the process shared such a core similarity with iPSC technology, which provides a potential explanation and natural origin for the mechanism that the scientific community has harnessed to great effect," said first author Brian Lin, a Ph.D. graduate of the Sackler School of Graduate Biomedical Sciences at Tufts and now a postdoctoral fellow at Mass General Hospital.
"The direct restoration of adult stem cells has implications for many types of tissue degeneration associated with aging, though we are several years away from designing actual therapies based on this work. The olfactory epithelium is a singularly powerful model for understanding how tissues regenerate or fail to do so," said senior author Jim Schwob, M.D./Ph.D., a professor of Developmental, Molecular & Chemical Biology at Tufts University School of Medicine in Boston.
"If we can restore the population of stem cells in the olfactory epithelium by regenerating them or by administering the right drug as a nasal spray, we may be able to prevent deterioration in the sense of smell," he continued.
More information: Brian Lin et al, Injury Induces Endogenous Reprogramming and Dedifferentiation of Neuronal Progenitors to Multipotency, Cell Stem Cell (2017). DOI: 10.1016/j.stem.2017.09.008



















