Rare melanoma type highly responsive to immunotherapy
Desmoplastic melanoma is a rare subtype of melanoma that is commonly found on sun-exposed areas, such as the head and neck, and usually seen in older patients. Treatment is difficult because these tumors are often resistant to chemotherapy and lack actionable mutations commonly found in other types of melanoma that are targeted by specific drugs. However, Moffitt Cancer Center researchers report in the Jan. 10 issue of Nature that patients with desmoplastic melanoma are more responsive to immune-activating anti-PD-1/PD-L1 therapies than previously assumed.
Drugs that reactivate a patient's own immune system to target cancer cells are rapidly changing the face of cancer therapy. Pembrolizumab and nivolumab have been approved to treat melanoma, and others are in development. These drugs block the interaction between the proteins PD-1 and PD-L1. During cancer development, PD-1 and PD-L1 inhibit the immune system and allow tumor cells to escape detection and continue to grow. By blocking their interaction, immune-activating drugs restimulate the immune system to detect and destroy cancer cells.
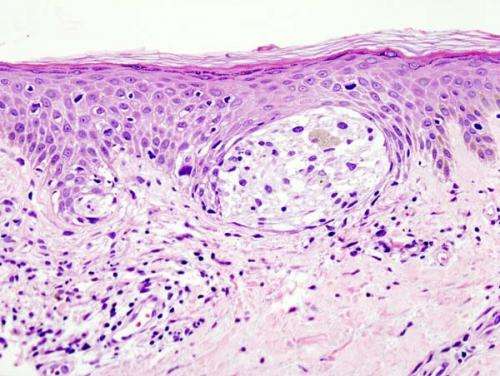
Scientists previously believed that the tissue architecture of desmoplastic melanomas would reduce the ability of immune cells to infiltrate the tumor area and limit the effectiveness of immune-activating drugs. However, based on anecdotal reports of favorable responses, a group of researchers including Moffitt's Zeynep Eroglu, M.D., Jane Messina, M.D., and Dae Won Kim, M.D., hypothesized that patients with desmoplastic melanoma may be more responsive to anti-PD-1/PD-L1 therapies than previously assumed, and explored this in the largest group of immunotherapy-treated desmoplastic melanoma patients studied to date.
To test their hypothesis, the researchers analyzed 60 patients with advanced/metastatic desmoplastic melanoma who were previously treated with a drug that targets either PD-1 or PD-L1. They discovered that 42 patients had a significant response to treatment. Approximately half of these patients had a complete response in which their tumors entirely disappeared, and the remainder had a partial response, with significant reduction of their tumors. Seventy-four percent of patients were still alive more than two years after beginning treatment. This 70 percent response rate is one of the highest reported for anti-PD-1/PD-L1 therapies to date, and is even higher than response rates commonly observed in patients with other subtypes of melanoma, which are approximately 35 to 40 percent.
In a collaborative effort involving 10 United States and international cancer centers including Moffitt and University of California Los Angeles, researchers wanted to determine the biological reasons why patients with desmoplastic melanoma may benefit from drugs that target PD-1 or PD-L1. They first confirmed that desmoplastic melanomas have high levels of DNA mutations, as they are highly associated with ultraviolet light DNA damage caused by sun exposure. NF-1 mutations were found as the most common driving genetic event. They also demonstrated that desmoplastic melanomas have the pre-existing immune cells and proteins necessary to mount an immune response against cancer cells. They compared tissue biopsies from patients with desmoplastic melanoma and non-desmoplastic melanoma. They discovered that desmoplastic melanomas have more cells with high levels of the PD-L1 protein within both the tumor and the invading edges of the tumor. Desmoplastic melanomas also have high levels of immune cells called CD8 T cells that are critical for immune-activating drugs to be effective.
"Our findings challenge the previous school of thought that immunotherapy would offer little benefit to patients with desmoplastic melanoma due to the dense tissue architecture of these tumors. These tumors in fact have the necessary biological ingredients to be very effective targets for anti-PD-1 drugs," said Eroglu, assistant member of the Cutaneous Oncology Department at Moffitt. "Often, combinations of two immunotherapy drugs are used to treat patients with melanoma to try to improve tumor response rates and survival above current reported rates. However, these combinations can lead to significantly higher rate of severe side-effects than treatment with anti-PD-1 therapy alone. Our data suggest that single-agent anti-PD-1 therapy may well be sufficient for patients with desmoplastic melanoma, potentially sparing them the increased toxicities generally observed with combinations of immunotherapies."
More information: Zeynep Eroglu et al, High response rate to PD-1 blockade in desmoplastic melanomas, Nature (2018). DOI: 10.1038/nature25187
















