Scientists identify immune cascade that fuels complications, tissue damage in chlamydia infections
Closing a critical gap in knowledge, Harvard Medical School scientists have unraveled the immune cascade that fuels tissue damage and disease development in chlamydia infection—the most common sexually transmitted disease in the United States.
Physicians have long known that complications of chlamydia are not caused by the bacterium itself but instead arise from inflammation in the reproductive organs. However, up until now, it remained unclear what drives this damaging inflammation.
Findings of the new research, conducted in mice and published Feb. 9 in PNAS, reveal the precise mechanism behind this phenomenon and identify the cast of immune cells involved in it. Further, the research shows that the body deals with chlamydia infection via two distinct and separate immune pathways—one driving the clearance of bacteria and one fueling inflammation and tissue damage.
More than 2.8 million chlamydia infections occur each year in the United States, according to the Centers for Disease Control and Prevention. Left untreated, chlamydia can lead to pelvic inflammatory disease, chronic pelvic pain, ectopic pregnancy, infertility and prostate inflammation. Chlamydia infections can be cleared with prompt antibiotic treatment, but most people infected with the bacterium have silent infections, resulting in delayed treatment. Untreated infections that linger for months—and sometimes for years—can cause irreversible inflammatory damage to the reproductive organs.
"By the time the infection is identified, irreversible damage has often occurred so we urgently need therapies that prevent these devastating consequences," said senior author Michael Starnbach, professor in the Department of Microbiology and Immunobiology at Harvard Medical School. Our findings offer a roadmap for the development of vaccines that can stimulate immune protection against chlamydia-associated diseases."
The study findings show that complications of chlamydia infections arise from inflammation that occurs when several types of protective immune cells rush to the reproductive organs after the bacterium invades the body. Remarkably, the research shows these immune cells are not involved in the clearance of bacteria, but rather that clearance is instead prompted by a different class of immune cells.
The existence of such separate immune responses is good news, the researchers said.
"This is a truly encouraging finding," said study first author Rebeccah Lijek, who conducted the research as a post-doctoral fellow at Harvard Medical School and is now assistant professor of biological science at Mount Holyoke College. "It means that if one class of immune cells is responsible for clearing the infection, while another class of immune cells causes tissue damage and subsequent disease, then we can develop treatments that precision target inflammation without exacerbating bacterial levels."
To understand how the bacterium damages urogenital tissue, the team started out by recreating symptoms that mimic human chlamydia infection in mice—the first successful instance of doing so. Past failures to replicate human symptoms in an animal model have hampered the understanding of the chlamydia-driven diseases for decades, the team said.
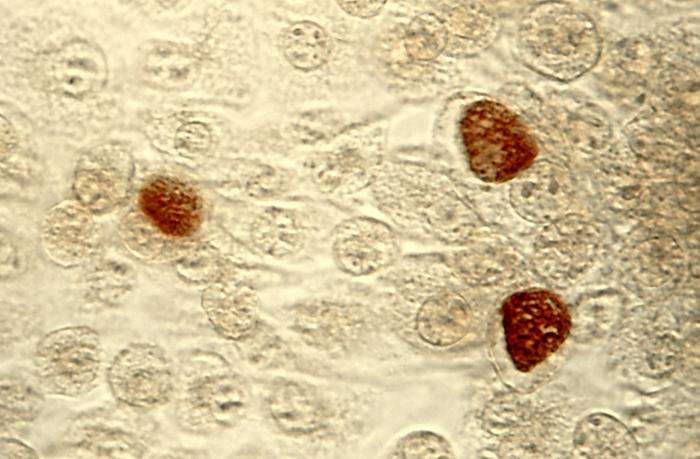
Next, the team analyzed the reproductive tissue of infected mice, using a technique that identifies the presence of various immune cells. The researchers observed that in the first few days after infection, immune cells known as neutrophils—the body's first responders—charge up to the urogenital tract and cause inflammation and damage. To determine what happens in the absence of neutrophils, researchers used an antibody specifically designed to target these cells while sparing all others. Chlamydia-infected mice that lacked neutrophils showed no tissue damage despite harboring the bacterium. The absence of neutrophils had no effect on bacterial levels—an indicator that neutrophils play no role in the clearing of the bacterium.
Further analysis showed that in the later stages of infection—a week or so after the bacterium enters the body—a different set of immune cells make their way to the urogenital tract. Researchers observed dramatically elevated levels of two types of T cells. Known as the body's elite assassins, T cells are "trained" to seek out and destroy pathogens. In this case, however, researchers identified two distinct subtypes of T cells: general-assignment, bystander T cells that drive inflammation and chlamydia-specific T cells, formed in response to the presence of this particular bacterium. Previous research conducted by Starnbach's team had shown that chlamydia-specific T cells are responsible for clearing the infection but up until now the scientists didn't know whether the chlamydia-specific T cells might also spark damaging inflammation. They do not, the study showed.
To understand what drives inflammation-inducing cells to infected urogenital tissue, researchers analyzed more than 700 inflammation-promoting and immunity-inducing genes. During infection, these genes release signaling proteins known as chemokines, which call on immune cells to make their way to the site of infection. Researchers identified a trio of chemokines—CXCL 9,10,11—that were particularly elevated, compared with all others. These very proteins are also known to play a role in the autoimmune conditions inflammatory bowel disease and rheumatoid arthritis.
In a final step, the researchers used a chemical compound to block the activity of the inflammation-inducing chemokines. Mice treated with the compound had markedly reduced levels of nonspecific, bystander T cells and markedly less inflammation and tissue damage, compared with untreated mice. Notably, the improvement occurred without any effect on bacterial levels.
Several compounds that target the receptor for inflammation-inducing chemokines CXCL 9,10,11 are currently being tested in clinical trials as a treatment for inflammatory bowel disease.
"Our data suggest that such therapies may also be beneficial in the treatment and prevention of pelvic inflammation following chlamydia infection," Lijek said.
More information: Rebeccah S. Lijek et al. Pathology afterChlamydia trachomatisinfection is driven by nonprotective immune cells that are distinct from protective populations, Proceedings of the National Academy of Sciences (2018). DOI: 10.1073/pnas.1711356115


















