Scientists make white blood cells to alleviate pain during tissue inflammation in mice
Researchers at the University of Granada led a novel study in mice that shows that sigma‑1 receptor blockers cause white blood cells or leukocytes to relieve pain when a tissue is inflamed
Immune system cells (leukocytes or white blood cells) accumulate in the tissues, for example, after suffering a trauma or a wound. Their main function is repairing the damaged tissue. However, in addition to that function, those cells release substances that produce pain (called algogenic chemicals), playing a key role in the pain felt when the tissue is inflamed. This is also applicable to certain chronic pathologies that present inflammation and pain, as is the case of arthritis.
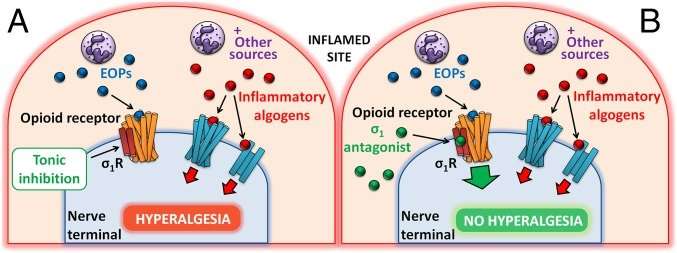
Paradoxically, these leukocytes, in addition to releasing algogenic chemicals, are capable of producing endogenous opioid peptides (such as endorphins). These peptides have the same activity as opioid analgesics used for treating pain. However, the balance between the analgesic and the pain‑inducing activity of leukocytes during inflammation clearly favors pain; in fact, inflammation produces pain.
The sigma‑1 receptor is a very small protein present in neurons, and is capable of modulating the action of opioid receptors. A study led by scientists from the University of Granada (UGR) has discovered that sigma‑1 receptor blockers are capable of increasing the effect of endogenous opioid peptides produced by leukocytes, so that these cells relieve pain instead of producing it when they are in the inflamed tissue.
"We present a totally novel pain relief mechanism, based on maximizing the analgesic potential of the immune system cells, and which could have important therapeutic applications in patients with pain of inflammatory origin", says the director of this work, professor Enrique J. Cobos del Moral, researcher from the Department of Pharmacology and the Institute of Neuroscience of the University of Granada.
More information: Miguel A. Tejada et al. Sigma-1 receptors control immune-driven peripheral opioid analgesia during inflammation in mice, Proceedings of the National Academy of Sciences (2017). DOI: 10.1073/pnas.1620068114
















