COVID-19 vaccines could go to children first to protect the elderly
The World Health Organization is discussing how best to allocate and prioritize COVID-19 vaccines when they arrive.
It is focusing on the immediate crisis. To reduce deaths quickly when there are extremely limited vaccine doses available, vaccinating older, more vulnerable people is expected to be the best option, even if the vaccine is relatively poor at protecting them. That is because the elderly are so much more likely to die from the disease.
But as we produce more vaccines, the goal will be returning to normality where we can freely mix without increased risk. If vaccines are not very effective in older adults, we will need many more people to be vaccinated, including children. One possible strategy is to prioritize children.
Why children first?
The risks and benefits of particular COVID-19 vaccination strategies depend on information we don't yet have. For example, we don't yet know whether vaccines work or are safe for specific population groups, such as the young or the old.
But it is worth thinking about the ethics of different strategies in advance. In a pandemic, time can save lives.
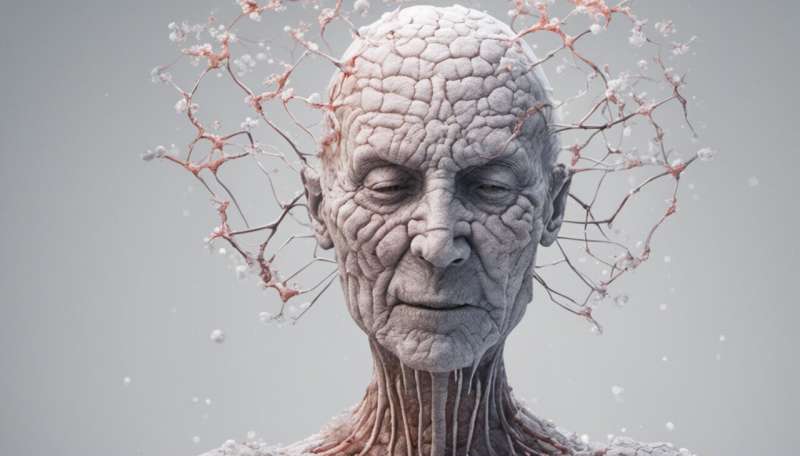
A COVID-19 vaccine may be less effective in the elderly because their immune systems decline naturally with age, making them perhaps less able to trigger an efficient, protective immune response after vaccination.
We see this with the flu vaccine, which only reduces influenza-like illnesses by around one-third in the over-65s and deaths by around half.
If there are similar results for a COVID-19 vaccine, to return to normality, we may need to also prevent community transmission through vaccinating young people, who generally mount a stronger immune response. This would in turn protect older, more vulnerable people because the virus would be less likely to reach them.
Yes, this is controversial. Children cannot autonomously consent to being vaccinated. Adults, who make these decisions on their behalf, are also likely to benefit from a reduced risk of contracting the virus within their own household, making the decision a possible conflict of interest.
When would this be OK?
We do sometimes make altruistic decisions on behalf of children. Children can be life-saving bone marrow donors for siblings, for example, despite the risks.
We can also apply the idea that we can restrict liberty where there is a risk of harm to others. For instance, if a child is infected with COVID-19, they need to be isolated and quarantined just like adults.
However, vaccination differs from both examples in one key respect. With vaccination, there is unlikely to be a single identified person the child will help, or whom they are uniquely placed to help. Instead, the potential benefits are collective, to the wider public.
If a child lived with a sibling who had an underlying condition that makes them particularly vulnerable to COVID-19, or lived with their grandparents, vaccination might be an easier choice.
Three factors could help us decide
When weighing up whether children should be vaccinated ahead of adults, we can ask:
1. How severe is the threat to public health?
So far, more than a million people have died from COVID-19. There's also the risk of overwhelming health systems and the additional collateral damage in terms of economic, social, educational and risk of excess non-COVID-19 deaths as a result (for example through suicide, or delayed access to health care). COVID-19 affects everyone in society, including children.
2. Are there alternatives?
If vaccination works well enough in vulnerable people, or there are other strategies to achieve the same effect, such as general adult vaccination, we should use those instead.
3. Is the response proportional to the threat?
As we vaccinate the vulnerable, and the general adult population, even if it is not fully effective, we will reduce the severity of the crisis. We should assess at that stage whether the remaining problem warrants vaccinating children.
Assuming we meet these conditions, we argue prioritizing childrens' vaccination, on a voluntary basis at least, is the right strategy.
How about mandatory vaccinations?
Mandatory vaccination can be justified if voluntary strategies do not achieve herd immunity, or do not achieve it fast enough to protect the vulnerable.
To gage whether mandatory vaccination is worth it, we might also need to consider how lethal and infectious a virus is.
For instance, smallpox had a death rate of up to 30% (although contagion requires fairly prolonged contact). It was eradicated by 1979 through vaccination, which was mandatory in many countries. With COVID-19, 0.1-0.35% of infections are fatal.
By definition, mandatory vaccination involves some form of coercion. This can include withholding financial benefits or access to early childhood education (No Jab, No Pay or No Jab, No Play in Australia); preventing children from entering school (U.S., with specific rules varying by state) to fines (Italy). France even has legal provision for imprisonment for parents who refuse certain vaccines.
Mandatory vaccination (of some kind) could be justified in groups who are at increased personal risk from COVID-19—such as health-care workers, the elderly, men, or people with other health conditions—if incentives such as increased freedoms, or even payment are not sufficient. For these groups, the vaccine is win-win: it both protects others and the person vaccinated.
And mandatory vaccinations for children?
The situation is more tricky with children. Unless they have underlying health conditions or have a rare but serious inflammatory condition after infection, children are less likely to have severe COVID-19 or die from it.
So the risk of the vaccine itself (as yet unknown) weighs more heavily.
On the other hand, children benefit from grandparent relationships, and other freedoms afforded by a pandemic-free society.
Mandatory vaccination might be justified in children if the following criteria are met:
- the vaccine is proven to be very safe for children (including in the long term, as yet unknown), and safer than the effects of the disease
- children are significant spreaders of infection (which does not appear to be the case for COVID-19, at least for pre-teens)
- there are other non-COVID benefits to children, such as return to normal social and educational life (school), and access to normal health-care services which they otherwise could not have
- measures are reasonable and proportionate, for instance, by limiting child care benefits (rather, for instance, than sending parents to prison).
We are certainly not close to meeting these criteria for mandatory vaccination of children against COVID-19 yet, especially as we don't know how effective and safe candidate vaccines are in different populations.
This article is republished from The Conversation under a Creative Commons license. Read the original article.![]()





















