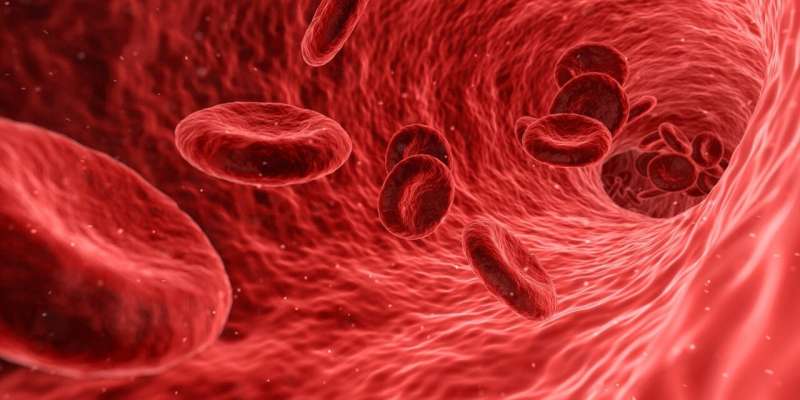
Q&A: Blood disorder causes body to make too many red blood cells
DEAR MAYO CLINIC: I have a relative who was diagnosed with polycythemia vera. What is this disorder, and can it be treated? Is any new research being conducted on polycythemia vera?
ANSWER: Polycythemia vera is a blood disorder where the body makes too many red blood cells. It's one in a family of diseases called myeloproliferative disorders. In these diseases, bone marrow—the spongy tissue inside bones where blood cells are made—is affected by a type of chronic leukemia that causes it to make more cells than it should.
Patients with polycythemia vera have a high red blood cell count. But sometimes the disease also can result in too many white blood cells, or too many platelets—the component of blood that aids in clotting. A considerable amount of research is underway to investigate this blood disorder and treatments for it.
Exactly why polycythemia vera develops is still unclear, although researchers know more about the cause of the disease now than in the past. In 2005, researchers found that a change in a gene that affects the protein JAK2 appears to play a role in polycythemia vera development.
JAK2 is one in a series of on/off switches that control when cells grow and divide. In polycythemia vera, this switch is stuck in the on position, causing cell growth to continue. About 95% of people with polycythemia vera have the JAK2 mutation. The others have different mutations that are thought to affect cells similarly. Research is ongoing.
In its early stages, polycythemia vera may not cause symptoms. Due to the excess red blood cells, though, some people may eventually develop skin itchiness and redness; headaches; dizziness; shortness of breath; and numbness, tingling, burning or weakness in their hands, feet, arms or legs. Because polycythemia vera causes blood to thicken and slow, it also can increase the risk of developing blood clots, which can cause a stroke.
Over the long term, polycythemia vera may progress to myelofibrosis, a disorder that involves scarring in the bone marrow and disruption of the production of blood cells, and it can lead to enlargement of the spleen and liver. Polycythemia vera also can progress to acute leukemia, a cancer of the blood and bone marrow.
Treatment of polycythemia vera focuses on controlling symptoms and decreasing the risk of blood clots or bleeding. Therapies often include a daily dose of aspirin and reducing the amount of red blood cells by periodically drawing blood from a vein.
In some high-risk patients, medication may be used to decrease the number of red blood cells or to suppress the bone marrow's ability to produce blood cells. People who require medication typically include those older than 60, people who have previously had blood clots or bleeding, people who are at high risk of heart disease, and those with significantly elevated platelet counts.
The three main drugs used to treat polycythemia vera and lower blood counts have been hydroxyurea, peginterferon alfa-2a and ruxolitinib. Hydroxyurea is the typical first therapy, as it works well and has the least side effects. Ruxolitinib is unique in that it targets the JAK2 mutation directly. The most recently approved drug is ropeginterferon alpha 2b-njft. It was approved in November 2021. It also works to reduce red blood cell production and decrease the risk of blood clots. Patients who progress to myelofibrosis or acute leukemia may need chemotherapy, a bone marrow stem cell transplant or both to treat the disease.
Over 250 clinical trials are being conducted on polycythemia vera. The research includes new drugs, as well as therapies for controlling symptoms and reducing the risk of progression to myelofibrosis and acute leukemia.—Dr. Marwan Shaikh, Hematology/Oncology, Mayo Clinic, Jacksonville, Florida
2022 Mayo Clinic News Network.
Distributed by Tribune Content Agency, LLC.

















