This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Marker for therapy response in acute myeloid leukemia identified
With the combination of the drugs Venetoclax and 5-Azacitidine, a new, effective and more tolerable alternative to chemotherapy for the treatment of AML has been available for several years. But for some patients, the drug combination does not work.
Doctors and scientists from the German Cancer Research Center, the Heidelberg Stem Cell Institute HI-STEM and Heidelberg University Hospital have now developed a marker for therapy response: Only when leukemia stem cells express a specific combination of cell death-inhibiting proteins do patients respond to the new therapy.
Acute myeloid leukemia (AML) is the most common and very aggressive form of blood cancer in adults. Until recently, only high-dose chemotherapy was available to treat the disease. But for about half of those affected, especially elderly or frail individuals, this distressing treatment is out of the question.
The agent Venetoclax has been approved for several years. The survival of AML cells depends on certain proteins that suppress programmed cell death—apoptosis. Venetoclax specifically inhibits the anti-apoptotic protein BCL-2, which leukemia cells use to protect themselves from cell death, thereby keeping AML in check. A combination of Venetoclax and the epigenetic drug 5-Azacitidine (Ven/Aza) is comparatively well tolerated and has significantly improved the treatment of patients for whom high-dose chemotherapy is not an option.
Therefore, it is currently being investigated whether this drug combination is also suitable as a so-called first-line treatment in younger or physically fit AML patients, which would spare them the need for high-dose chemotherapy. However, not every AML patient responds to the drug combination. In some cases, the leukemia cells are resistant from the start.
"Until now, there have been no predictive markers that can reliably predict a response to Venetoclax," says Andreas Trumpp, head of department at the German Cancer Research Center (DKFZ) and director of HI-STEM in Heidelberg.
Together with colleagues from Heidelberg University Hospital, Alexander Waclawiczek, Aino-Maija Leppä and Simon Renders in the Trumpp team now looked for characteristics in blood and bone marrow samples from Ven/Aza-treated AML patients that correlate with response to therapy.
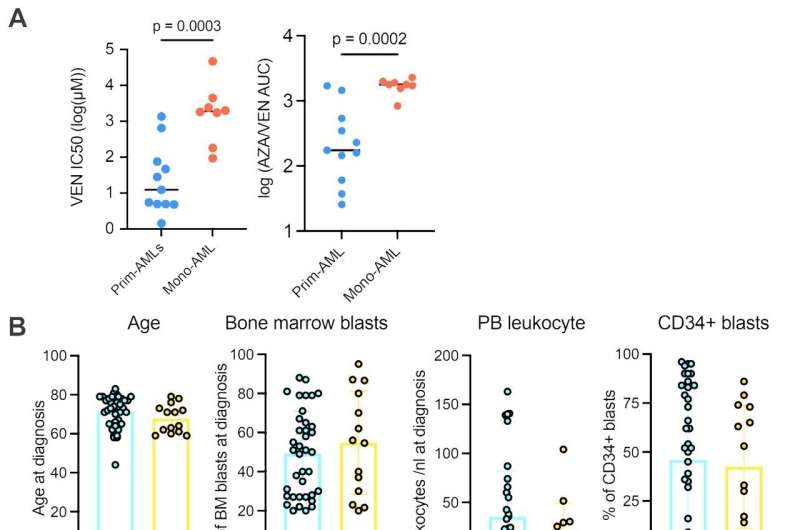
The researchers found that a small population of cells that exhibit characteristics of leukemia stem cells is responsible for therapy response. If these cells express a specific combination of proteins in the BCL-2 family, the Ven/Aza combination can trigger programmed cell death in the leukemia stem cells, halting AML.
BCL-2, a known inhibitor of apoptosis, is a member of a family of proteins involved in the regulation of programmed cell death. The Heidelberg research team found that it is not only the amount of BCL-2 in the leukemia stem cells that determines the Ven/Aza response, but that it is the quantitative ratio of certain members of the BCL-2 family that is important.
Based on this observation, they derived the so-called "MAC score" ("Mediators of Apoptosis Combinatorial score"), which expresses the quantity ratio of the proteins BCL-2, BCL-xL and MCL-1 in the AML stem cells and can be determined by flow cytometry. The higher the score, the longer the treatment success lasted.
"We can thus provide an inexpensive test that gives reliable information after just a few hours as to whether an AML is responding to Ven/Aza and thus whether the stressful high-dose chemotherapy can be avoided," says study leader Andreas Trumpp. "The test can be performed in any well-equipped hematology laboratory to determine the best possible form of treatment for leukemia patients."
The study is published in the journal Cancer Discovery. Together with Carsten Müller-Tidow at Heidelberg University Hospital V, the results will be further evaluated in prospective clinical studies before the test can find its way into the routine care of AML patients.
More information: Alexander Waclawiczek et al, Combinatorial BCL-2 family expression in Acute Myeloid Leukemia Stem Cells predicts clinical response to Azacitidine/Venetoclax, Cancer Discovery (2023). DOI: 10.1158/2159-8290.CD-22-0939

















