This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
New study links gum disease to buildup of Alzheimer's plaque formation
Although most people don't associate oral disease with serious health problems, increasing evidence shows that oral bacteria play a significant role in systemic diseases like colon cancer and heart disease. Now, new research from the Forsyth Institute shows a link between periodontal (gum) disease and the formation of amyloid plaque, a hallmark of Alzheimer's disease.
In their paper, "Microglial cell response to experimental periodontal disease," published in the Journal of Neuroinflammation, Forsyth scientists and their collaborators at Boston University demonstrate that gum disease can lead to changes in brain cells called microglial cells, which are responsible for defending the brain from amyloid plaque. This plaque is a type of protein that is associated with cell death, and cognitive decline in people with Alzheimer's. The study provides important insight into how oral bacteria makes its way to the brain, and the role of neuroinflammation in Alzheimer's disease.
"We knew from one of our previous studies that inflammation associated with gum disease activates an inflammatory response in the brain," said Dr. Alpdogan Kantarci, senior member of staff at Forsyth and a senior author of the study. "In this study, we were asking the question, can oral bacteria cause a change in the brain cells?"
The microglial cells the researchers studied are a type of white blood cell responsible for digesting amyloid plaque. Forsyth scientists found that when exposed to oral bacteria, the microglial cells became overstimulated and ate too much. "They basically became obese," Dr. Kantarci said. "They no longer could digest plaque formations."
The finding is significant for showing the impact of gum disease on systemic health. Gum disease causes lesions to develop between the gums and teeth. The area of this lesion is the size of your palm. Dr. Kantarci explained, "It's an open wound that allows the bacteria in your mouth to enter your bloodstream and circulate to other parts of your body." These bacteria can pass through the blood/brain barrier and stimulate the microglial cells in your brain.
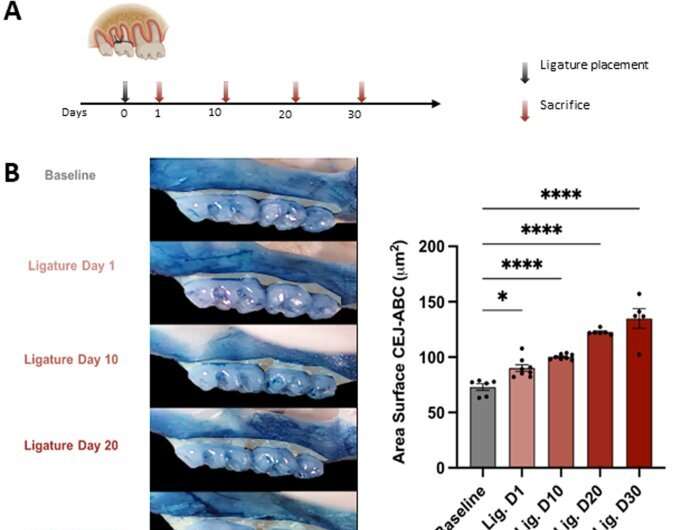
Using mouse oral bacteria to cause gum disease in lab mice, the scientists were able to track periodontal disease progression in mice and confirm that the bacteria had traveled to the brain.
They then isolated the brain microglial cells and exposed them to the oral bacteria. This exposure stimulated the microglial cells, activated neuroinflammation, and changed how microglial cells dealt with amyloid plaques.
"Recognizing how oral bacteria causes neuroinflammation will help us to develop much more targeted strategies," said Dr. Kantarci. "This study suggests that in order to prevent neuroinflammation and neurodegeneration, it will be critical to control the oral inflammation associated with periodontal disease. The mouth is part of the body and if you don't take care of oral inflammation and infection, you cannot really prevent systemic diseases, like Alzheimer's, in a reproducible way."
This study is the first time that scientists caused periodontal disease with mouse-specific bacteria and could study the effects of same-species oral microbiome on the brain. Having same-species bacteria and cells brings the test closer to replicating what the process looks like in humans.
The research team consisted of Rawan Almarhoumi, Carla Alvarez, Theodore Harris, Bruce J. Paster, and Alpdogan Kantarci of Forsyth, and Christina M. Tognoni, Isabel Carreras, and Alpaslan Dedeoglu of Boston University.
More information: Rawan Almarhoumi et al, Microglial cell response to experimental periodontal disease, Journal of Neuroinflammation (2023). DOI: 10.1186/s12974-023-02821-x



















