This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Strengthening artificial immune cells to fight cancer
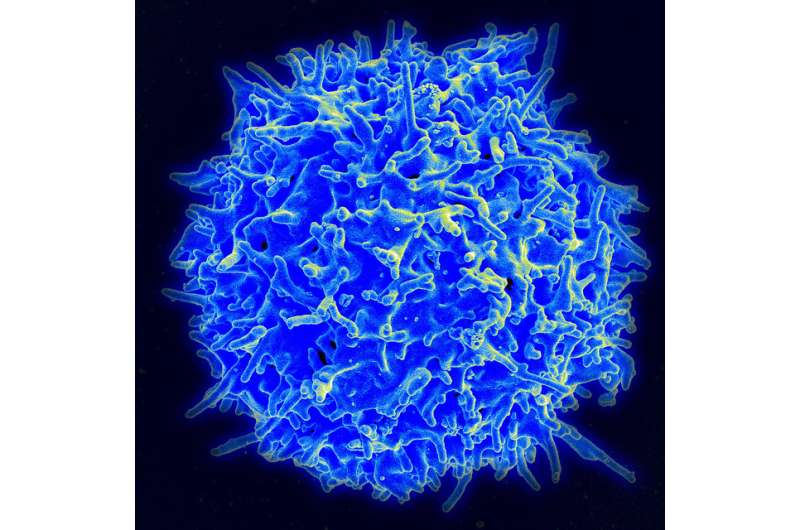
Among available immunotherapies, the use of CAR T cells is proving extremely effective against certain blood cancers, but only in half of patients. A main reason for this is the premature dysfunction of these immune cells, which have been artificially modified in vitro.
A team from the Universities of Geneva (UNIGE), Lausanne (UNIL), the Geneva University Hospitals (HUG) and the Vaud University Hospital (CHUV), all part of the Swiss Cancer Center Léman (SCCL), has discovered how to prolong the functionality of CAR T cells. By inhibiting a very specific metabolic mechanism, the team has succeeded in creating CAR T cells with enhanced immune memory, capable of fighting tumor cells for much longer. These very promising results are published in the journal Nature September 20, 2023.
CAR T cell immunotherapy involves taking immune cells—usually T lymphocytes—from a person suffering from cancer, modifying them in the laboratory to increase their ability to recognize and fight tumor cells, then readministering them to the patient. However, as with other types of immunotherapies, many patients do not respond to the treatment or relapse.
"CAR T cells must be massively multiplied before they can be administered," explains Mathias Wenes, a research fellow who coordinated this research in the laboratory of Pr Denis Migliorini, Department of Medicine at the UNIGE Faculty of Medicine and Department of Oncology at HUG. "But the disease history of the patient, in combination with the amplification process, exhausts the cells: they reach a state of terminal differentiation that precipitates the end of their life cycle without leaving them time to act on the length."
A mechanism common to cancer cells and immune cells
In the absence of oxygen, cancer cells resort to a very specific survival mechanism: they metabolize the amino acid glutamine as an alternative source of energy through a chemical reaction known as "reductive carboxylation."
"Immune cells and cancer cells have a fairly similar metabolism, which enables them to proliferate very rapidly. We have indeed discovered here that T cells also used this mechanism," explains Alison Jaccard, a Ph.D. student in Professor Ping-Chih Ho's laboratory in the UNIL-CHUV Department of Oncology and the study's first author.
To investigate the role of reductive carboxylation, the scientists inhibited this mechanism in CAR T cells in mouse models of leukemia and multiple myeloma, two blood cancers. "Our modified CAR T cells multiplied normally and did not lose their capacity to attack, indicating that reductive carboxylation is not essential for them," Wenes sums up.
Mice cured with CAR T cells
In addition, the mice treated in this way were virtually cured of their cancer, a result well beyond the research team's expectations. "Without reductive carboxylation, the cells no longer differentiate as much and maintain their anti-tumor function for longer. And even, and this is the heart of our discovery, they tend to transform into memory T lymphocytes, a type of immune cell that retains the memory of the tumor elements that needs to be attacked."
Memory T lymphocytes play a key role in the secondary immune response. They retain the memory of pathogens previously encountered and can reactivate when its reappears—as in the case of a virus, but also in the case of tumor pathogens—providing much longer-lasting immune protection. "The same principle applies to CAR T cells: the higher the number of memory cells, the more effective the anti-tumor response and the better the clinical outcome. The state of differentiation of CAR T cells is therefore a key factor in the success of the treatment."
A cross-talk between metabolism and gene expression
Unfolded, the DNA contained in each of our cells would measure about two meters in length. To fit into the tiny cell nucleus, it is condensed around proteins called histones. In order for gene transcription to occur, specific DNA regions need to unwrap, which happens by modifying histones.
When T cells are activated, histone modifications take place which, on one hand, condense DNA and prevent transcription of genes ensuring longevity, while on the other hand open up and allow transcription of genes driving their inflammatory and killing function. Reductive carboxylation acts directly on the generation of metabolites, small chemical elements that modify histones, to influence DNA packaging and to prevent accessibility to longevity genes. Its inhibition maintains the opening of those genes and promotes their transformation into long-lived memory CAR Ts.
The inhibitor used by the scientists to block reductive carboxylation is a drug already approved for the treatment of certain cancers. "We therefore propose to reposition it in order to extend its use and produce more powerful CAR T cells in vitro. Of course, their efficacy and safety need to be tested in clinical trials, but we have very good hopes," conclude the authors.
More information: Mathias Wenes, Reductive carboxylation epigenetically instructs T cell differentiation, Nature (2023). DOI: 10.1038/s41586-023-06546-y. www.nature.com/articles/s41586-023-06546-y



















