This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Study highlights gut fungi's lasting impact on severe COVID-19 immune response
Certain gut-dwelling fungi flourish in severe cases of COVID-19, amplifying the excessive inflammation that drives this disease while also causing long-lasting changes in the immune system, according to a new study led by investigators at Weill Cornell Medicine and NewYork-Presbyterian. This discovery identifies a group of patients who may benefit from specialized, but yet-to-be determined treatments.
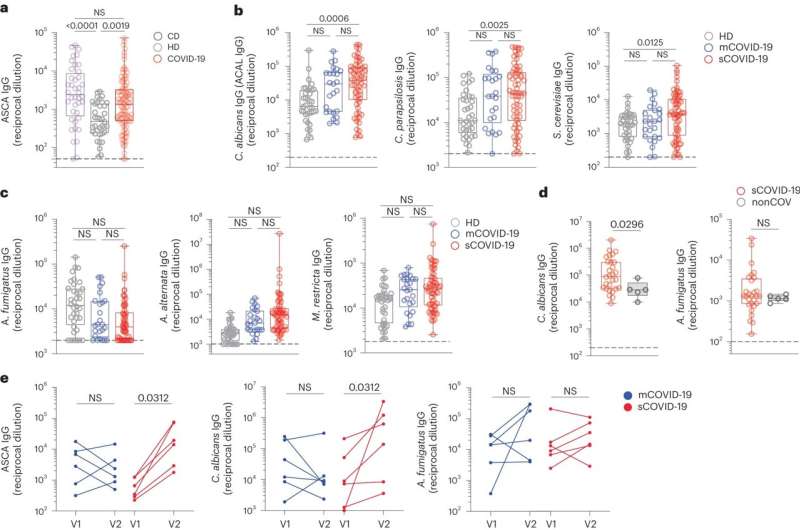
Utilizing patient samples and preclinical models, the research team determined that the growth of fungi in the intestinal tract, particularly strains of Candida albicans yeast, trigger an upsurge in immune cells whose actions can exacerbate lung damage. Their findings, published in Nature Immunology, also elucidate that patients retain a heightened immune response and immune memory against these fungi for up to a year after the resolution of SARS-CoV-2 infection.
The research reveals a new dimension of the complex pathology unleashed by severe COVID-19, according to senior author Dr. Iliyan Iliev, an associate professor of immunology in medicine in the Department of Medicine, co-director of the Microbiome Core Lab and a member of the Jill Roberts Institute for Research in Inflammatory Bowel Disease at Weill Cornell Medicine.
"Severe and long COVID-19 were not thought to involve fungal blooms in the intestines that, in addition to the virus, can impact patient's immunity," he said.
Dr. Iliev, an immunologist who studies the microbiome and the chronic inflammatory conditions targeting the gastrointestinal tract, pivoted to COVID-19 during the pandemic. As researchers gained a better handle on the new viral infections, it became clear that, in COVID-19 as in inflammatory bowel disease, the body's own inflammatory immune response causes harm.
To investigate this errant immune response, Dr. Iliev and Dr. Takato Kusakabe, a postdoctoral fellow and a first author in the study, worked with numerous colleagues to acquire three large clinical cohorts of COVID-19 patients and develop a mouse model to study the disease.
They collaborated with members of the Weill Department of Medicine and the Department of Pathology and Laboratory Medicine at Weill Cornell Medicine, including Dr. Stephen Josefowitz, Dr. Mirella Salvatore, Dr. Melissa Cushing, Dr. Lars Westblade, and Dr. Adolfo García-Sastre, a professor of microbiology and director of the Global Health and Emerging Pathogens Institute of the Icahn School of Medicine at Mount Sinai.
How gut fungi harm the lungs
The team first made the connection when analysis of blood samples from patients at New York-Presbyterian/Weill Cornell Medical Center diagnosed with severe COVID-19 unveiled the presence of antibodies tuned to attack fungi common to the gut. The researchers then found that populations of yeast, and one species in particular, Candida albicans, increased in the intestines of the patients during the course of severe COVID-19.
When they looked at the patients' immune systems, the researchers found a parallel increase in immune cells called neutrophils. In severe COVID-19, excessive numbers of neutrophils appear in the lungs, where their activity worsens the inflammatory response already damaging these organs.
Turning to preclinical models, the investigators found that mice bearing fungi from patients with severe COVID-19 produced more neutrophils in their blood and lungs, and had signs of heightened inflammation when infected with SARS-CoV-2. However, giving them an antifungal drug reduced these effects.
The immune system remembers
From within patients' blood samples, researchers also uncovered evidence of persistent changes to the immune system they believe are related to a condition known as long COVID-19, in which symptoms linger, or new ones develop, after an infection has cleared.
When the team examined patients' blood up to a year afterward, they found it still contained anti-fungal antibodies. In addition, when they looked at the stem cells that give rise to neutrophils, the researchers found that these progenitors are primed to respond to fungi. They found that an immune protein called IL-6 that these fungi induce, appears to bolster both the neutrophils and the antibodies.
Further experiments showed that blocking IL-6 in the patients or in mice dampened this immunological memory, causing the presence of neutrophils and antibodies to wane.
While these results do not have immediate implications for treating severe or long COVID-19, they suggest new opportunities to tailor therapy, according to Dr. Iliev. For example, anti-fungal antibodies could potentially serve as a marker to identify patients who might benefit from a therapy that targets the fungi or the immunological changes they instigate.
Or, assuming further research supports it, the antibodies' presence could indicate someone might be at risk for long COVID-19. The team's discoveries may also have relevance beyond COVID-19, said Dr. Iliev, who notes this research could open new avenues of exploration for the treatment of other infectious and inflammatory diseases.
More information: Takato Kusakabe et al, Fungal microbiota sustains lasting immune activation of neutrophils and their progenitors in severe COVID-19, Nature Immunology (2023). DOI: 10.1038/s41590-023-01637-4 www.nature.com/articles/s41590-023-01637-4
Katherine Lagree et al, Candida makes a lasting impression in COVID-19, Nature Immunology (2023). DOI: 10.1038/s41590-023-01648-1 , doi.org/10.1038/s41590-023-01648-1


















