This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Obesity-cancer connection discovery suggests strategies for improving immunotherapy
Immune system cells called macrophages play an unexpected role in the complicated connection between obesity and cancer, a Vanderbilt University Medical Center-led research team has discovered.
Obesity increases the frequency of macrophages in tumors and induces their expression of the immune checkpoint protein PD-1—a target of cancer immunotherapies. The findings, published June 12 in the journal Nature, provide a mechanistic explanation for how obesity can contribute to both increased cancer risk and enhanced responses to immunotherapy. They may also suggest strategies for improving immunotherapy and for identifying patients who will respond best to such treatments.
"Obesity is the second leading modifiable risk factor for cancer, behind only smoking, and obese individuals have a greater risk for worse outcomes. But they also can respond better to immunotherapy," said Jeffrey Rathmell, Ph.D., Cornelius Vanderbilt Professor of Immunobiology and director of the Vanderbilt Center for Immunobiology.
"How is it that there can be this worse outcome on one hand, but better outcome on another? That's an interesting question."
Postdoctoral fellow Jackie Bader, Ph.D., led the studies to examine the influence of obesity on cancer and to explore this "obesity paradox"—that obesity can contribute to cancer progression but also improve response to immunotherapy.
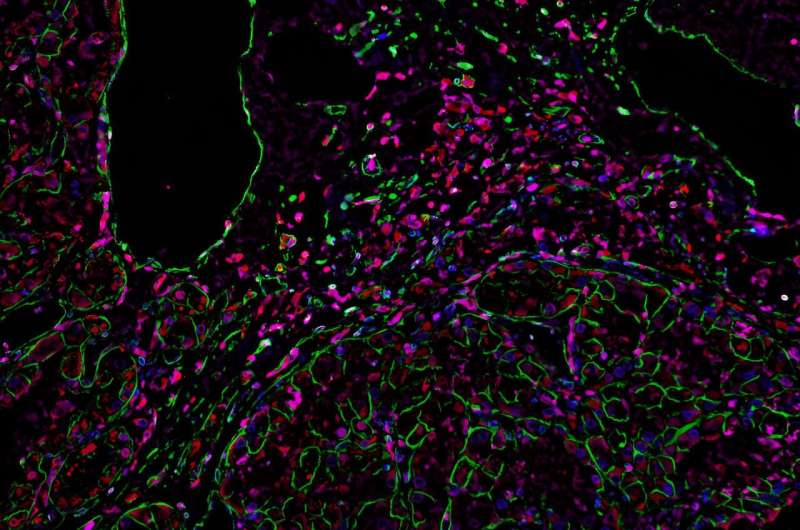
In a mouse model, the researchers found striking differences between the macrophages isolated from tumors in obese versus lean mice. While the protein PD-1 is an immunotherapy target normally thought to act on T cells, they discovered that the macrophages in tumors from obese mice expressed higher levels of PD-1, and that PD-1 acted directly on the macrophages to suppress their function.
In tumor samples from patients with kidney cancer, the researchers also found PD-1-expressing macrophages, and in human endometrial tumor biopsies from patients before and after 10% weight loss, they showed that PD-1 expression on tumor-associated macrophages decreased following weight loss.
"We were very fortunate to have collaborators that provided us with samples from the same patients before and after weight loss that reinforced the findings from our mouse models," Bader said.
Blocking PD-1 with an immunotherapy drug in the mouse models increased tumor-associated macrophage activity, including their ability to stimulate T cells.
Cancer immunotherapy studies have largely focused on T cells, because they are the immune cells that can kill cancer cells, Bader and Rathmell said. But macrophages play important roles in influencing what T cells do.
"I've always been 'team macrophage,'" Bader said. "Macrophages are thought of as being like a garbage truck: They clean up the mess. But they have a huge spectrum of activity to enhance the immune response, and they're more plastic and manipulatable than other immune cells, which makes them really interesting."
The presence of more macrophages expressing PD-1 in tumors in an obese setting provides a mechanistic explanation for the obesity paradox, Bader and Rathmell said. Increased PD-1 expression suppresses immune surveillance by macrophages—and subsequently suppresses the killer T cells—allowing tumors to grow (the increased cancer risk of obesity).
PD-1 blockade with immunotherapy allows the increased number of PD-1-expressing macrophages to act (the enhanced response to immunotherapy).
Currently, immune checkpoint inhibitors work in only 20–30% of patients.
"We clearly want to find ways to make immunotherapies work better, and in the obese setting, they naturally work better," Rathmell said. "Understanding how these processes are working biologically may give us clues about how to improve immunotherapy in general."
The findings also suggest that examining levels of PD-1-expressing tumor macrophages may help identify patients who will respond better to immunotherapy.
"It could be that the greater the proportion of PD-1-expressing macrophages a tumor has, the better the response to immunotherapy will be," Rathmell said.
More information: Jeffrey Rathmell, Obesity induces PD-1 on macrophages to suppress anti-tumor immunity, Nature (2024). DOI: 10.1038/s41586-024-07529-3. www.nature.com/articles/s41586-024-07529-3


















