This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Shoring up blood vessels may offer new approach for treating autoimmune rheumatic diseases
A study from physician-scientists at the Hospital for Special Surgery (HSS) points to a potential novel approach for treating autoimmune diseases like rheumatoid arthritis—preventing antibodies and immune cells from leaving the bloodstream and entering joints and other organs where they cause inflammation and injury. The findings were published on June 10 in JCI Insight.
Current treatments for autoimmune diseases focus on suppressing the parts of the immune system that trigger inflammation and cause disease symptoms. But the immune-suppressing activity of these drugs also leads to side effects, including an increased susceptibility to infections.
New therapies are needed that are anti-inflammatory without being immunosuppressive. The new study suggests that if immune cells and autoantibodies can be kept within the bloodstream, inflammatory damage is prevented.
"The idea is that if we can bolster the integrity of the blood vessels, we can prevent the immune components that trigger and mediate inflammation from entering tissues and attenuate disease," says first author Nathalie Burg, MD, a rheumatologist and assistant scientist in the HSS Research Institute.
"This would be a completely new approach to treat or prevent organ damage in autoimmune diseases," adds senior author Jane Salmon, MD, a rheumatologist and senior scientist at HSS.
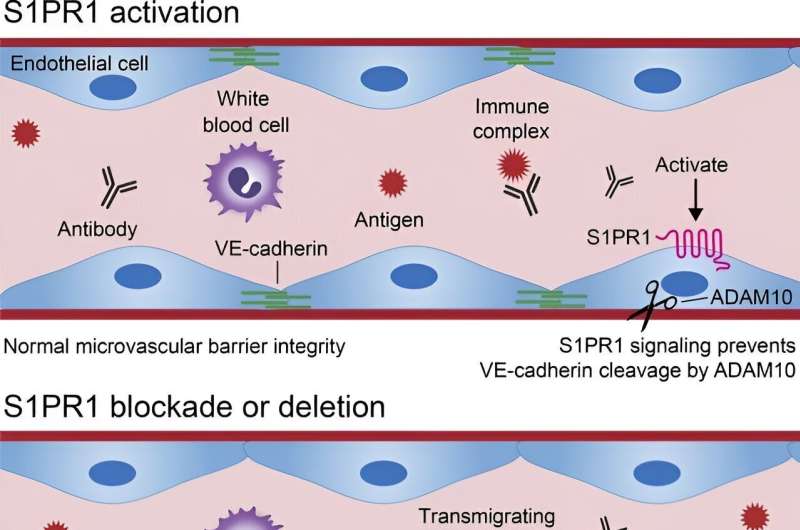
The key to this research is a molecule called S1PR1 (sphingosine 1-phosphate receptor 1). S1PR1 is important for maintaining vascular integrity—meaning it helps the endothelial cells lining the walls of the blood vessels stick together.
As part of the study, the scientists first developed mouse models with S1PR1 knocked out specifically in endothelial cells and determined that when these mice were exposed to serum that causes arthritis, there was more inflammation and damage in their joints.
In contrast, drugs that augment S1PR1 signaling and tighten the junctions between endothelial cells attenuated arthritis in experimental models. Subsequently, an analysis of samples from patients with rheumatoid arthritis confirmed decreased levels of S1PR1 in the microvessel endothelial cells lining the joints as well as lower levels of S1P and Sa1P, molecules that stimulate S1PR1, circulating in the bloodstream.
"This helps to confirm the role that S1PR1 plays," Dr. Salmon explains.
While doing this research, Dr. Burg also discovered a mechanism by which S1PR1 regulates the integrity of the blood vessel walls: It helps to restrain the cleavage of a molecule called VE- cadherin, which acts like Velcro in holding the endothelial cells together. Thus, when S1PR1 is deleted or its function is blocked, the VE cadherin molecules are broken and the blood vessels become leaky.
"This research is truly multidisciplinary and also unconventional," Dr. Salmon says. "It represents the capacity to apply one field—vascular biology—to another—immunology. It is really done at the interface of the two disciplines." Dr. Burg learned many of the techniques used in this research in the laboratory of Timothy Hla, Ph.D., a leading vascular biologist and investigator at Harvard Medical School. Dr. Hla and members of his team are co-authors of the paper.
The investigators plan to continue studying this approach, with the goal of designing clinical trials of drugs that boost endothelial cell S1PR1. Such drugs already exist.
Drs. Burg and Salmon posit that these interventions would likely be used in combination with existing drugs, especially in early disease, before longstanding damage has occurred.
"We don't think this pathway is powerful enough to prevent these diseases on its own, but by combining this type of drug with an immunosuppressant, we might get a synergistic effect," Dr. Burg says.
"This might allow us to reduce the amount of immunosuppression that is needed to keep autoimmune disease under control. We are testing the role of endothelial S1PR1 in other models of inflammatory arthritis."
More information: Nathalie Burg et al, Endothelial cell sphingosine 1-phosphate receptor 1 restrains VE-cadherin cleavage and attenuates experimental inflammatory arthritis, JCI Insight (2024). DOI: 10.1172/jci.insight.171467


















