This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
proofread
Adjuvant therapy for hepatocellular carcinoma after curative treatment: Several unanswered questions
Hepatocellular carcinoma (HCC) is one of the most prevalent malignancies globally and is the third leading cause of cancer-related deaths. The primary curative treatments for HCC are liver transplantation, hepatectomy, and local ablation. However, the recurrence rate of HCC following hepatectomy or ablation remains alarmingly high, up to 70%, severely impacting patient prognosis and overall survival (OS).
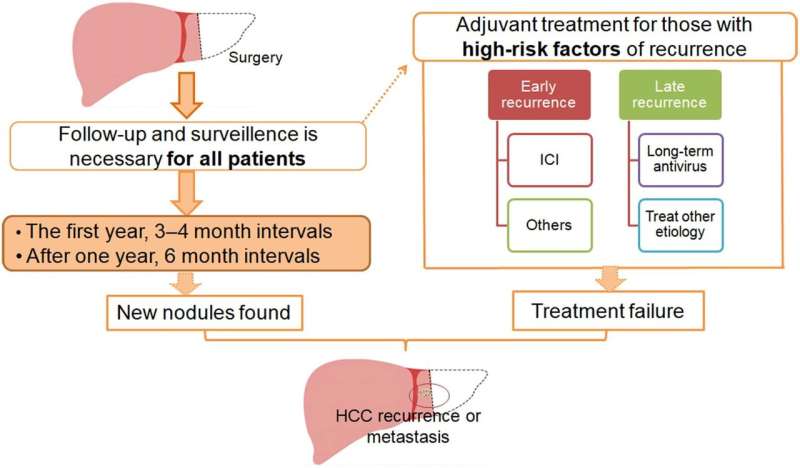
To mitigate postoperative recurrence and improve patient outcomes, various adjuvant therapies have been explored. Despite the efficacy of several adjuvant treatments in reducing recurrence rates and enhancing survival, there is no standardized consensus on their application across national guidelines, leading to significant disparities in recommendations between Eastern and Western medical practices.
HCC recurrence can generally be classified into two categories: early recurrence, which typically occurs within two years post-treatment, and late recurrence, which occurs after two years. Early recurrence is often linked to intrahepatic micrometastases or microthrombi from the primary tumor, whereas late recurrence is usually associated with multicentric new tumor formations.
Risk factors for early recurrence include large tumor size (>5 cm), multiple tumors, the presence of satellite lesions, lack of a tumor capsule, tumor rupture, non-anatomical resection, narrow resection margins (≤2 cm), high alpha-fetoprotein levels (≥400 ng/mL), and microvascular or macrovascular invasion. Conversely, late-recurrence risk factors include liver cirrhosis, higher hepatitis activity grades, and poor tumor classification.
The primary aim of adjuvant therapy following local treatments like hepatectomy or ablation is to reduce the recurrence rate and thus improve recurrence-free survival (RFS) and OS. The choice of adjuvant therapy should be guided by the risk factors specific to early or late recurrence.
- Antiviral therapy: For patients with hepatitis-related HCC, antiviral therapy aims to inhibit long-term viral replication, reduce liver damage, prevent disease progression, and ultimately prolong survival. For HCV-related HCC, sustained viral eradication using interferon-based or interferon-free regimens significantly reduces recurrence. Similarly, for HBV-related HCC, nucleos(t)ide analogs such as tenofovir and entecavir are recommended. Studies have shown that tenofovir is particularly effective in reducing recurrence and improving survival compared to entecavir.
- Transarterial chemoembolization (TACE): This is often used as an adjuvant therapy for patients at high risk of intrahepatic metastasis. TACE targets disseminated tumor cells that have spread from the primary tumor, helping to reduce early recurrence by effectively eliminating residual tumors.
- Immune checkpoint inhibitors (ICIs): Recent guidelines, particularly in the United States, have begun to include recommendations for ICIs in the adjuvant setting. ICIs help boost the body's antitumor immunity and have shown promise in reducing recurrence rates and improving survival outcomes in HCC patients.
Despite the promising results of various adjuvant therapies, there remain several unanswered questions and challenges. The lack of a universally accepted standard for adjuvant therapy in HCC highlights the need for further research and clinical trials to establish clear guidelines.
Moreover, the balance between the benefits and potential adverse effects of adjuvant treatments must be carefully considered to optimize patient outcomes. Future studies should aim to refine patient selection criteria for adjuvant therapies, tailoring treatments based on individual risk profiles to maximize efficacy and minimize harm.
In conclusion, while significant strides have been made in the development of adjuvant therapies for HCC, ongoing research and international collaboration are essential to standardize treatment protocols and improve the prognosis for HCC patients worldwide.
The study is published in the Journal of Clinical and Translational Hepatology.
More information: Le Li et al, Adjuvant Therapy for Hepatocellular Carcinoma After Curative Treatment: Several Unanswered Questions, Journal of Clinical and Translational Hepatology (2024). DOI: 10.14218/JCTH.2024.00030





















