How cervical cancer vaccines came to be
(HealthDay)—The cervical cancer vaccine has turned into one of the biggest success stories in the field.
Although almost a half-million women develop cervical cancer annually, health experts predict that number is likely to drop dramatically in the coming years because of two vaccines that can prevent many cases of the disease.
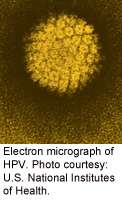
It wasn't until the 1980s that researchers confirmed that most cases of cervical cancer were caused by the human papillomavirus (HPV). The most common sexually transmitted virus, HPV has more than 40 different strains that can affect the genital area, according to the U.S. Centers for Disease Control and Prevention. Most people who are infected with HPV never know they've been infected.
"After the agent that causes cervical cancer was found to be HPV, the idea for a vaccine was obvious to many," said Dr. Alfred Saah, director of vaccines clinical research for Merck and Co., in Whitehouse Station, N.J. "The question then became which part of the virus was related to immunity and would be the best part of the virus to make a vaccine."
Saah said that work began in earnest in the early 1990s on cloning the relevant parts of the virus strains that would be needed for an effective vaccine. To prevent cervical cancer, the vaccine would need to teach the immune system to recognize the human papillomavirus cells so that it would respond by destroying those cells.
"The vaccine stimulates the body's immune system in several ways so that when the host is exposed to natural HPV, the immune system is ahead of the virus and neutralizes the virus before infection and disease can occur," Saah explained.
Once a potential vaccine was created, tests in animals showed it worked extremely well. Then, the vaccine had to pass phase 1 clinical trials in humans, which had to demonstrate that the vaccine causes the body's immune system to respond against the virus. Next up were phase 2 trials, which helped determine the lowest dose necessary to create an immune response.
Two large phase 3 trials followed, which Saah said together involved nearly 20,000 people. Their purpose was to assess both safety and efficacy.
Based on the positive results of these trials, the vaccine, which was developed by Merck and is now named Gardasil, was approved by the U.S. Food and Drug Administration in June 2006. Since that time, another HPV vaccine—Cervarix, made by GlaxoSmithKline—also has been approved to prevent cervical cancer.
"Gardasil was the first HPV vaccine specifically designed to prevent cervical cancer," Saah said. "It [targets] four HPV types: HPV 6 and 11, which cause 90 percent of genital warts, and HPV types 16 and 18, which cause 70 percent of cervical cancers." In addition to cervical cancer, HPV has also been linked to cancers of the anus, penis, vagina and vulva, and to some cancers of the throat, according to Saah.
More information: Read more about all of the cancer vaccines that are being researched.
Copyright © 2013 HealthDay. All rights reserved.















