December 3, 2013 report
Can inhaled stem cells fix your brain?
(Medical Xpress)—In certain neurosurgical procedures, like fixing pituitary glands, surgeons can remove a tumor through the nose with minimal damage to surrounding tissue. It turns out, that passing things in the other direction—into the brain through an intranasal route—has many advantages too. Everything from drugs, proteins, and gene vectors, to stem cells, can now by administered in this way. The major question for today, is not so much what do these agents do, but where do they go once they are inside? StemGenex, a La Jolla-based company, has recently announced their new hopes for a treatment which could potentially address several neurological diseases. They are now offering a therapy for patients with multiple sclerosis in based on the intranasal delivery of mesenchymal stem cells.
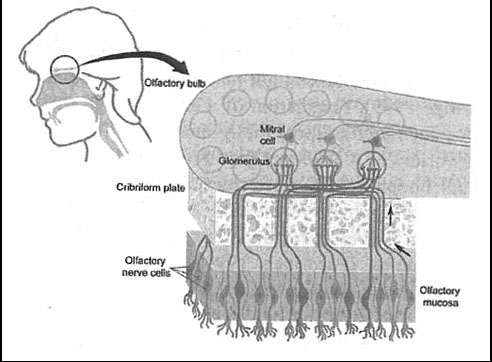
The preferred medical term for act of snorting is insufflation. While insufflation is an obvious choice to deliver drugs to the sinuses or lungs, it is now appreciated that many bioactive agents can get much further than that. One major advantage of this method is the low barrier of entry through the mucous membranes into the bloodstream. Although some pro-drugs, like codeine, require absorption through the gut to pass to the liver where they can be metabolized into an active form, many other drugs are compromised by a digestive passage. What's more important though here for the brain, is that the normally-intact blood brain barrier can by bypassed either by slipping around the perineural sheath cells, or getting endocytosed and retrogradely transported along either the olfactory nerves, or the trigeminal nerves.
While whole cells are not typically endocytosed into vesicles, there are less obvious ways that cells can get in, particularly in compromised or lesioned brains. In cultured cells, perhaps a lesioned brain by any standard, it has been clearly shown that embryonic stem cells readily fuse with microglia. These microglia then, in turn, go on to fuse with mature neurons. But definitively demonstrating that intranasally-delivered stem cells reach appropriate targets, and have restorative or therapeutic effect can be a little trickier. One study which looked at delivery of bone marrow-derived stromal (connective tissue) cells, in mice with a lesioned striatum thrown in for good measure, was able to detect an autofluorescence signal that was similar to the fluorescent protein label in the delivered cells—but a clear sign of the cells themselves was hard to establish.
Further studies are undoubtedly needed to definitively establish the fate of stem cells introduced to the brain by any method. For the treatment of tumors like glioblastoma multiforme, that which killed Ted Kennedy, intranasally-sourced stem cells may be used to provide a vehicle for the delivery of other agents, like TNF (Tumor Necrosis Factor). Some simpler treatments that have gotten recent attention include the even more-difficult-to-corroborate enhancement of brain function in autism through intranasal oxytocin.
Treatment of Parkinson's disease is another potential application. Animal models in which mesenchymal cells that presumably migrated into the brain, survived up to six months, and delivered dopamine to restore motor function have been reported previously. Some of these studies have been on the table a few years now though, and it is important to revisit them as other treatments and methods come along. As a final consideration, perhaps the most interesting offering to date has been a device for good old-fashioned intranasal neurophotobiostimulation. While this may sound fantastic, the designers may be on to something—if it can be used as the front end for the optogenetic treatments of the not so far future.
More information: www.prweb.com/releases/StemCel … MS/prweb11305257.htm
© 2013 Phys.org














