Two players produce destructive cascade of diabetic retinopathy
The retina can be bombarded by reactive oxygen species in diabetes, prompting events that destroy healthy blood vessels, form leaky new ones and ruin vision.
Now researchers have learned that those chemically reactive molecules must come from both the bone marrow as well as the retinal cells themselves to cause such serious consequences.
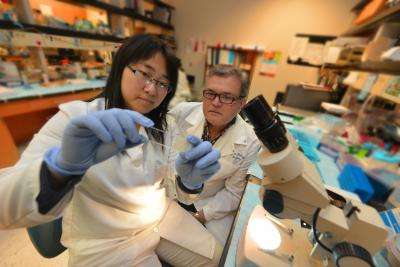
"It's a cascade that requires two players to signal the next event that causes the damage," said Dr. Ruth Caldwell, cell biologist at the Vascular Biology Center at the Medical College of Georgia at Georgia Regents University.
The good news is the finding also provides two new points for intervention, said Dr. Modesto Rojas, MCG postdoctoral fellow and first author of the study in the journal PLOS ONE.
Excessive glucose in the blood prompts excessive production of reactive oxygen species, or ROS, and the light-sensitive retina is particularly vulnerable. Caldwell's research team had previously documented that ROS from white blood cells produced by the bone marrow as well as from retinal cells were the major instigators in diabetic retinopathy, a leading cause of blindness worldwide. But they weren't sure which mattered most.
So they looked as several different scenarios, including mice lacking the ability to produce ROS by either the retinal or white blood cells, and found that if either were lacking, future damage was essentially eliminated. "One alone can't do it," said Caldwell, the study's corresponding author. "They did not develop the early signs of diabetic retinopathy that we were measuring."
While blocking ROS production by retinal cells could be difficult, drugs already exist that reduce activation of white blood cells. Those cells not only make ROS, but also adhere to blood vessel walls in the retina that become sticky in diabetes, Rojas said. In fact, a study published in October 2013 in PLOS ONE showed that neutrophil inhibitory factor could block the vascular lesions that are a hallmark of diabetic retinopathy without hurting the immunity of diabetic mice. The MCG scientists note that decreased activation does not impact the immune protection white blood cells also provide.
Next steps include studying those drugs in their animal models and learning more about how ROS causes the collateral damage that can destroy vision. "All of this is some sort of wound-healing response gone wrong," Caldwell said.
ROS, a natural byproduct of the body's use of oxygen, has healthy roles in the body, including cell signaling, but is destructive at high levels that result from disease states such as diabetes.



















