Blood vessels and the immune system talk to each other; implications for cancer treatment
Some cancer therapies aim at stopping tumor growth by affecting the blood vessels that nurture the tumor mass, while others act on the immune system attempting to eliminate the tumor. Researchers at Baylor College of Medicine have discovered that tumor blood vessels and the immune system influence each other's functions, and propose that considering these bilateral effects in cancer therapy might improve outcomes. The study appears in Nature.
"One of the characteristics of successful cancerous tumors is their ability to trigger the formation of new blood vessels, a process called angiogenesis, to supply oxygen and nutrients to the growing cell mass," said corresponding author Dr. Xiang Zhang, associate professor of molecular and cellular biology and the Lester and Sue Smith Breast Center at Baylor. "Therapies that aim at blocking angiogenesis to starve the tumor can retard its growth; however, they can also have an undesired effect, tumor progression and resistance to treatments."
To better understand this apparent contradiction, Zhang and colleagues have taken a closer look at the tumor microenvironment in breast cancer.
Blood vessels and the immune system talk to each other
"We are trying to uncover a more complete picture of the tumor microenvironment in breast cancer," said Zhang, who is also a McNair Scholar at Baylor. "The tumor environment includes tumor cells and other types of cells that are recruited to the tumor mass and help the tumor grow. Scientists have divided those cells into subpopulations and studied them separately. We think that for a more complete understanding of the entire tumor microenvironment we have to study it with all its cell types together. Here, we applied this approach and discovered for the first time connections between tumor blood vessels and the immune system."
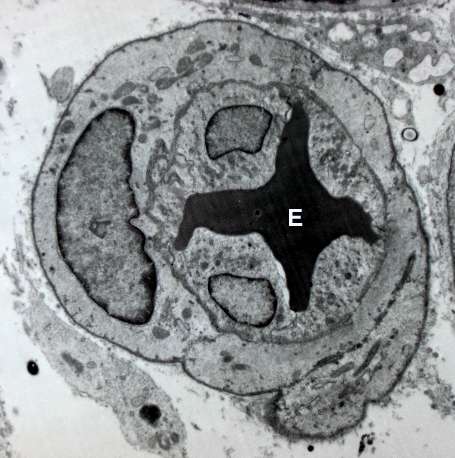
Despite their abundance, tumor blood vessels perform their job poorly because their structure and functions are abnormal. For instance, they do not carry enough blood to the tumor which limits the amount of oxygen and nutrients and creates a harsh microenvironment that can stimulate some cancer cells to escape through gaps in blood vessels and lead to metastasis. Abnormal tumor blood vessels may also interfere with anti-tumor immune cells or drugs attempting to reach the tumor.
Recently, restoring tumor blood vessels' function and structure to normal, a process called vessel normalization, has been considered a promising strategy to improve anti-blood vessel therapies. Vessel normalization can potentially limit or prevent cancer progression and metastasis, and improve the response to immunotherapy, chemotherapy and radiation therapy. However, little is known about how the tumor microenvironment regulates vessel normalization.
By applying their approach of studying the tumor microenvironment as a whole, Zhang and his colleagues discovered that immune cells called T lymphocytes can promote the process of vessel normalization.
"The reciprocal regulation is also true," Zhang said. "If we change the structure of the vasculature of the tumor toward vessel normalization, then we can also stimulate T cells to infiltrate the tumor. This bidirectional regulation between blood vessels and the immune system had not been elucidated before."
Implications for cancer therapy
"Both anti-blood vessel therapies and immunotherapies have been used in the clinic and have different degrees of success," said Zhang. "For instance, immunotherapy has been successful in some types of cancer such as melanoma and lung cancer, which are very aggressive cancers that did not have effective treatment until these therapies came along. However, there are still many patients who do not respond to this type of therapy. Similarly, from the anti-blood vessel therapy we know that many attempts have not been as successful as anticipated, and we have not been able to understand why."
The researchers work suggests that therapies should consider not only, for instance, the presence of immune cells and their activities in the tumor microenvironment, but also the vascular structure of the tumor because it has implications of whether the tumor would be able to respond to immunotherapy.
"Our finding suggests that anti-cancer therapies toward the blood vessels most likely influence the anti-tumor immune response, and vice-versa. Therefore, there is a possibility that by combining the therapies we can achieve better outcomes," Zhang said. "However, we are still far from having practical clinical solutions. We hope that our work will provide some therapeutic theoretical basis for those researchers using the two different therapies to collaborate and look at each other's biomarkers and therapeutic strategies."
More information: Lin Tian et al, Mutual regulation of tumour vessel normalization and immunostimulatory reprogramming, Nature (2017). DOI: 10.1038/nature21724

















