Study suggests ways to manipulate T cell migration in autoimmune or inflammatory disease
To eradicate pathogens or counteract inflammation, cells of the immune system move through often rapid blood flow toward peripheral disease sites, such as skin, gut or lung. Thus a goal of immunologists has been to define the repertoire of molecules that not only keep fast-moving immune cells on course but allow them to access inflamed tissues.
Now, a team led by La Jolla Institute for Allergy and Immunology (LJI) researcher Klaus Ley, M.D., reports that helper T cells move toward inflamed tissue using membrane protrusions that stabilize them and provide traction on the vasculature. Using high-resolution microscopy and global molecular analysis, the team shows that immature T cells lack these protrusions but that maturing T-cells switch on a gene expression program to create material to construct them.
That work, published in the Dec. 26. , 2017, issue of Cell Reports, provides a brand new collection of factors potentially useful to modulate immune responses in conditions as diverse as cancer and autoimmune disease.
"Immature T cells remain in lymphoid organs and can't move into sites of infection," says Ley, a professor and head of in LJI's Division of Inflammation Biology. "To reach their targets, T cells must first acquire biomechanical properties necessary for migratory behavior. We now know they do that in part by deploying strategies similar to those we previously discovered in cells called neutrophils."
Specifically, in a 2012 Ley's group reported in Nature that white blood cells called neutrophils throw out tube-like protrusions to anchor themselves and avoid being swept away by blood rushing by at high speed. As neutrophils gently roll along, tether after tether is peeled loose and slung forward like a lasso to gain new traction and slow them down. The new work shows multiple types of mature T cells, which unlike neutrophils are part of the adaptive immune system, also sprout tethers and slings to help them migrate to targets. Those T cells include so-called Th1 and Th17 T helper cells, which "help" other cells mount an immune response, and regulatory cells called Tregs.
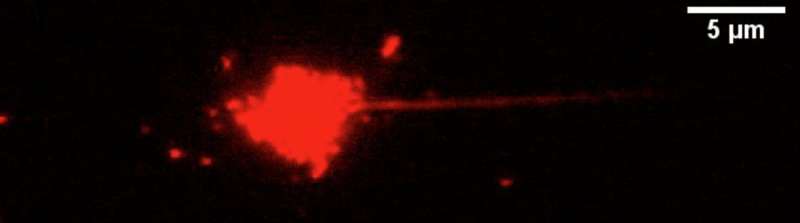
The group used microscopy to film these events using T cells engineered to harbor a fluorescent marker. The result was high-resolution videos of mature, red-glowing T cells rolling across either artificial surfaces or through living mouse muscle. The films, which were acquired using a microscopy technique Ley's group developed in 2010 and called quantitative dynamic footprinting nanoscopy, show that even under rapid fluid flow mature T cells manage to lay down multiple tethers and then swing them forward. By contrast, immature T cells remained devoid of protrusions and rolled poorly, apparently incapable of this type of cellular rappelling.
Extending protrusions apparently allows helper T cells to roll stably, regulate their speed, and then migrate into inflammatory sites. That protrusions are necessary for this fundamental behavior immediately suggests clinical applications—namely, that T cell responses could be either improved or impaired by manipulating how well a cell navigates the vasculature.
That possibility is bolstered by the fact that the new study also reports that, like their mouse cell counterparts, mature human T cells sprout comparable "tether and sling-like" protrusions to roll stably over surfaces.
Finally, to identify factors that could be exploited in T cell-based therapies, the group conducted global analysis of genes switched on or off as naive T cells acquired tether-and-sling-forming capacity. Several thousand genes showed changes in expression as naive T cells matured into migrating cells, and the Ley lab is now actively investigating the ones most directly involved in protrusion-formation.
"Many of these genes encode factors that make up a cell's internal framework, or cytoskeleton, or participate in cell invasion," says Ley. "This makes sense, for if cells put out cables to hold them in place, the cables must contain protein structures necessary for their integrity. Knocking out those proteins could arrest T cell migration."
The Ley lab is already using a target identified in the current analysis to write the story's next chapter, one relevant to psoriasis. Psoriasis is an autoimmune skin condition, which, like most autoimmune diseases, emerges in part when T cells become inappropriately mobilized to attack one's own tissue. "In the screen, we found a cytoskeletal protein upregulated in migrating T-cells," says Ley. "We already have evidence suggesting that if you interfere with that protein, psoriasis is less severe." This promising candidate identified in mouse studies will be the subject of future studies aimed at human disease.
Clinically, the converse is also possible, as illustrated by immunotherapy designed to rev up a patient's immune system to fight cancer. "Cytotoxic T cells and T helper cells are now being engineered to eradicate tumors," Ley says. "Our work suggests that additional manipulation of gene expression in those T cells could increase treatment efficacy by boosting homing to tumor tissue. These approaches require more work to determine which genes are essential for high-efficiency rolling, tether formation and immune cell recruitment."



















