Nerve cells found to suppress immune response during deadly lung infections
When the body is fighting infection, the immune system kicks into high gear. But emerging evidence hints at the involvement of another, rather surprising, player in this process: the nervous system.
New research from Harvard Medical School, conducted in mice, shows just how the interaction between the nervous and the immune systems occurs in deadly lung infections—a tantalizing clue into a complex interplay between two systems traditionally viewed as disconnected.
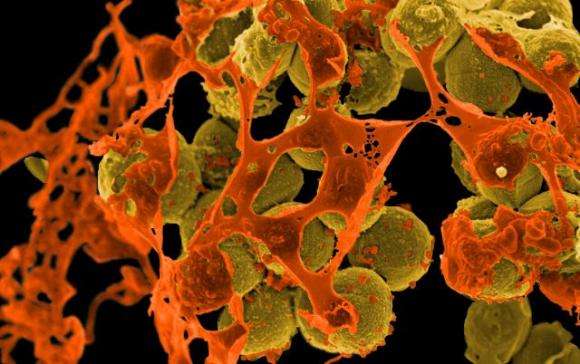
The findings, published March 5 in Nature Medicine, reveal that neurons carrying nerve signals to and from the lungs suppress immune response during infection with Staphylococcus aureus, a bacterium that is growing increasingly impervious to antibiotics and has emerged as a top killer of hospitalized patients, who are often immunocompromised and weakened overall.
The results, the researchers said, suggest that targeting the nervous system could be one way to boost immunity and can set the stage for the development of nonantibiotic approaches to treat recalcitrant bacterial infections.
"With the rapid emergence of drug-resistant organisms, such as methicillin-resistant Staph aureus, nonantibiotic approaches to treating bacterial infections are sorely needed," said senior study investigator Isaac Chiu, assistant professor in the Department of Microbiology and Immunobiology at Harvard Medical School.
"Targeting the nervous system to modulate immunity and treat or prevent these infections could be one such strategy."
Sensory neurons play a protective role by sensing adverse stimuli and alerting the body that something is awry. In the lungs, the neurons' projections detect mechanical pressure, inflammation, temperature changes and the presence of chemical irritants, then send an alert to the brain—a notification that can come in the form of pain, airway constriction or a cough that expels harmful agents or particles from the airways.
But the new study reveals that when mouse lungs are invaded by staph bacteria, these guardian neurons interfere with the organ's ability to cope with infection. Specifically, they reduce the lungs' ability to summon several types of disease-fighting cells in response to infection. A series of experiments conducted in mice revealed that disabling these neurons promoted immune cell recruitment, increased the lungs' ability to clear bacteria and boosted survival in staph-infected mice.
The results, the researchers said, suggest that different classes of sensory neurons may be involved in restraining or promoting immune response. Another possibility is that certain pathogens may have evolved to hijack and exploit an immunosuppressive pathway to their benefit—a survival mechanism for some classes of infectious bacteria, said study co-author Stephen Liberles, professor of cell biology at Harvard Medical School.
The team's interest in the crosstalk between the immune and nervous systems stems from recent work conducted by Chiu and colleagues. Chiu's earlier research showed that when nerve cells detect bacterial invaders, they produce pain during infection. Other research has revealed nervous system involvement in animal models of allergic asthma.
The team suspected that nerve cells would play a protective role in bacterial infections by boosting immune response to shield the lungs, but the experiments revealed the exact opposite. Much to their surprise, the scientists found that neurons dampened lung immunity and worsened outcomes in mice with bacterial pneumonia.
To determine how nerve cells affect immunity, the scientists genetically or chemically disabled lung neurons and then compared the activity of several types of immune cells involved in infection protection. They also monitored animal survival and took physiological measures such as body temperature and number of bacteria in the lungs.
In an initial set of experiments, researchers injected mice—half with intact neurons and half with chemically disabled neurons—with drug-resistant staph bacteria. Compared with mice with intact nerve receptors, mice with disabled neurons controlled their body temperatures better, harbored 10 times fewer bacteria in their lungs 12 hours after the infection and were markedly more capable of overcoming and surviving the infection. Sixteen of 20 mice with intact neurons succumbed to the infection. By contrast, 17 of 18 mice with disabled neurons survived.
The lungs of mice with genetically or chemically disabled neurons were also better at recruiting neutrophils—the body's pathogen-fighting troops that provide first responses during infections by devouring disease-causing bacteria. These mice summoned nearly twice as many infection-curbing neutrophils as did mice with intact neurons. But neutrophils in these animals were not simply more numerous. They were also more agile and more efficient in their performance. As a measure of agility, researchers compared how well neutrophils in both groups managed to patrol lung blood capillaries—a key ability that allows these cells to scan for the presence of disease-causing pathogens. Neutrophils in animals with chemically disabled neurons crawled farther, covering greater distances. They were also stickier and thus more capable of adhering to the walls of blood vessels, the site of their pathogen-gobbling action.
"We observed a striking difference in neutrophil presence and behavior between the two groups," said Pankaj Baral, a research fellow in microbiology and immunobiology at Harvard Medical School and first author on the study. "Neutrophils in mice with disabled neurons were simply better at doing their job."
Additionally, mice with disabled neurons marshaled more efficiently several types of cytokines, signaling proteins that regulate inflammation, infection and bacterial clearance. In animals with disabled neurons, the levels of these inflammatory cells ramped up and subsided much faster, indicating that these mice were capable of mounting a more rapid immune response in the early stages of infection.
Conversely, mice with intact neurons showed suppressed function in a class of protective immune cells known as gamma delta T cells, a type of protective white blood cell found mostly in barrier tissues that line a variety of organs, including the lungs.
A final set of experiments revealed just how neurons suppressed immunity. The researchers observed that an immune signaling molecule released locally by neurons—a neuropeptide known as CGRP—was markedly increased in mice with intact neuron receptors during infection but absent in mice with disabled neurons. Researchers observed that the release of this molecule interfered with the lungs' ability to summon immunoprotective neutrophils, cytokines and gamma delta T cells. Experiments in lab dishes revealed that CGRP disrupted immune cells' ability to kill bacteria. When researchers blocked the production of CGRP in live animals infected with staph, these mice showed an enhanced ability to fight infection.
Taken together, these findings show that lung neurons enable the release of CGRP during lung infections and that blocking the activity of CGRP improves survival in bacterial pneumonia.
"The traditional delineation between nervous and immune systems is getting blurry and our findings underscore the idea that these two systems cross-talk to regulate each other's function," Chiu said. "As we move forward, immunologists should think more about the role of the nervous system, and neuroscientists should think more about the immune system."
More information: Nociceptor sensory neurons suppress neutrophil and γδ T cell responses in bacterial lung infections and lethal pneumonia, Nature Medicine (2018). nature.com/articles/doi:10.1038/nm.4501




















