No 'reservoir': Detectable HIV-1 in treated human liver cells found to be inert
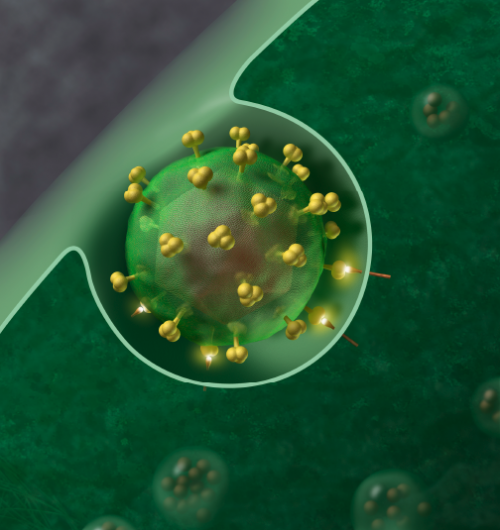
In a proof-of-principle study, researchers at Johns Hopkins report that a certain liver immune cell called a macrophage contains only defective or inert HIV-1 copies, and aren't likely to restart infection on their own in HIV-1-infected people on long-term antiretroviral therapy (ART).
The study, the investigators say, strongly suggest that defective or inert HIV-1 can remain in the liver macrophages for up to ten years without functioning as an HIV-1 "reservoir" that can replicate the virus at high levels.
But the finding, they say, also suggests that HIV-1 treatment strategies that only or mostly focus on these macrophages in a search for a cure might need to shift more heavily to other cell types more likely to serve as active reservoirs of the virus.
A report of the findings was published online on Sept. 10 and in the Oct. issue of the Journal of Clinical Investigation.
"Our study was the first, to our knowledge, in which purified liver tissue macrophages from HIV-1 infected people taking ART directly tested the idea that tissue macrophages are a long-lived active HIV-1 reservoir," says Ashwin Balagopal, M.D., an associate professor in the Division of Infectious Diseases at the Johns Hopkins University School of Medicine.
According to the U.S. Centers for Disease Control and Prevention (CDC), 36.7 million people worldwide and 1.1 million people in the U.S. are infected with HIV-1. Commonly, ART is successfully used to suppress the replication of HIV-1 and stop or control the progression of acquired immunodeficiency syndrome (AIDS) in humans. The virus infects the body's immune system cells, commonly forming a persistent, and reservoir in humans in so-called resting memory CD4+ T white blood cells. Macrophages work with T cells normally to envelop and clear tissues of microbes and debris.
The inability to completely wipe out pools of infectious HIV-1 has for decades frustrated efforts to completely cure the infection. And it means that the interruption or discontinuation of ART at any time re-activates HIV-1 replication, spreading the virus to new cells.
As a result, Balagopal says, investigators are increasingly focused more specifically on the location and biology of these HIV-1 reservoirs.
To determine if liver macrophages were a true source of infection-capable HIV-1 reservoirs after ART, liver tissue samples were taken from nine HIV-1 infected persons, seven of whom underwent liver transplantation at the Johns Hopkins Hospital and would have otherwise had their livers discarded. Eight of the nine persons were on ART for periods ranging from eight to 140 months.
The sample group included only adults whose demographic information is considered exempt from human subject research because all samples were obtained strictly for scientific reasons or postmortem, and would otherwise have been discarded. The Johns Hopkins School of Medicine institutional review approved this study protocol.
Using lab techniques that both measure HIV-1 containing T cells and separate out the liver macrophages, the researchers found HIV-1 to be present in the macrophages even after exposure to longstanding virus-suppressing ART.
However, Balagopal said that when his team tried to simulate virus "rebound" from the liver macrophages in the laboratory, they found only "fragments of HIV-1 in small quantities, without robust growth of full-length, infectious virus."
The researchers found that HIV-1 was in the liver macrophages of one subject who took ART for 11.7 years. They concluded that while liver macrophages might harbor HIV-1 for a long time, it's unlikely these viruses could continue an infection on their own, unlikely to function as a reservoir, because the viruses were not able to replicate.
Balagopal cautioned that their study results still affirm the need to address liver macrophage infection, because even if inert, these cells may be able to produce portions of viral proteins that can misdirect the immune system.
"These results contribute an important piece in our efforts to understand the role of non-T cells, such as macrophages, as HIV-1 cellular reservoirs in individuals on long-term ART, but also may help the research community focus on additional cure strategies," Abraham Kandathil, Ph.D., a research associate in the Division of Infectious Diseases at Johns Hopkins University School of Medicine who performed all of the key experiments.
In the future, Kandathil says, more research is needed to determine if the inert HIV-1 infected liver macrophages have any functional significance in people taking ART because expression of defective HIV-1 proteins can confuse the immune system and cause tissue inflammation.
"To find a comprehensive HIV-1 cure, it's important to identify all of the relevant HIV-1 reservoirs in the body, since it's possible that the virus hides in the DNA of numerous cell types and each may require different strategies to get a cure," says Balagopal.
Balagopal noted that their study was limited by the small number of liver macrophages and human samples studied, as well as the small number of CD4+ T cells in the liver cell cultures that may have prevented the researchers' ability to detect them.
More information: Abraham J. Kandathil et al, No recovery of replication-competent HIV-1 from human liver macrophages, Journal of Clinical Investigation (2018). DOI: 10.1172/JCI121678




















