Mechanism behind deadly fungal infection on top of influenza or COVID-19 deciphered
More than 15% of all critically ill patients who end up in intensive care with severe influenza or COVID-19 additionally develop aspergillosis, a pulmonary fungal infection. This doubles their mortality rate. A UZ Leuven and KU Leuven trial with international partners has revealed that multiple dysfunctions of the immune response lie at the basis of higher susceptibility to fungal infections. These insights were published in The Lancet Respiratory Medicine and constitute an important first step towards increasing the survival rate of patients with these severe lung infections.
Every year, hundreds of thousands of people worldwide end up in intensive care with influenza or COVID-19. About 15% of them develop an additional lung infection with the common fungus Aspergillus (aspergillosis). In healthy people, this infection hardly ever leads to illness. For critically ill patients with an underlying influenza or COVID-19 infection, however, aspergillosis can be deadly: the fungus can start to grow in the tissue of their respiratory tract and lungs and cause irreversible damage. The mortality rate of these patients becomes 40%–50%, about twice as high as that of ICU patients who only have severe influenza or COVID-19.
Compromised immune system
To find out why some patients with severe influenza or COVID-19 also develop aspergillosis and what to do about it, UZ Leuven and KU Leuven researchers set up an observational study, together with international colleagues. The study uncovered part of the mechanism that opens the door to an additional fungal infection in patients with an influenza or coronavirus infection.
Prof. Joost Wauters (UZ Leuven/KU Leuven), intensivist at UZ Leuven and the principal investigator of the study, explained, "We discovered that, in patients with serious influenza or COVID-19 who develop this type of fungal infection, the innate immune system had been affected in various areas. Their immune cells, which in healthy people are responsible for eliminating fungal spores in the lungs, were compromised. Furthermore, the white blood cells that would normally clean up fungal hyphae did not seem to function properly in those influenza or COVID-19 patients. It was surprising to see that partly similar deviating immune processes come into play in both COVID-19 and influenza."
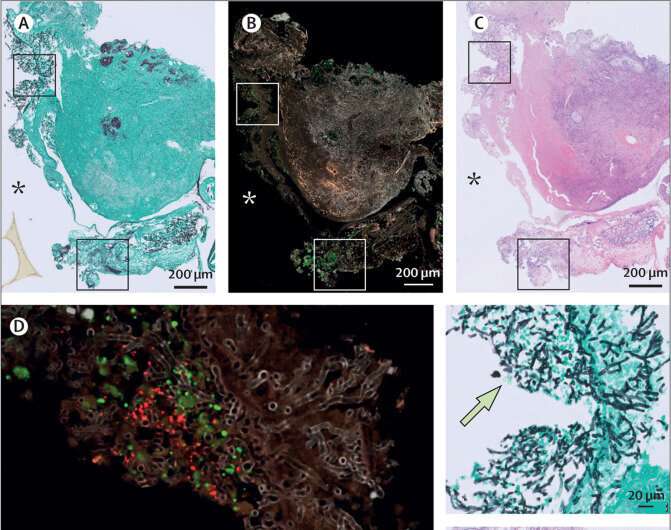
Dr. Simon Feys, internist in training at UZ Leuven and doctoral researcher at KU Leuven, added, "In tissue stainings, we also saw that the corona or influenza virus affects the epithelium of the lungs. This is the layer of cells that lines the respiratory tract and lung tissue, which forms the first barrier against infections. For COVID-19, we were able to show that specifically in the locations where the virus affects the epithelium, the fungus also penetrates the tissue."
Therapeutic target
Johan Van Weyenbergh (KU Leuven Rega Institute), Ph.D., who is the co-lead of the study, said, "With this information, we can develop biomarkers that help to predict which patients are more susceptible to a fungal infection and therefore need close follow-up."
Professor Agostinho Carvalho (University of Braga, Portugal), who also co-led the study, added, "Our results also lead the way for further research into medication that can repair the affected processes of the immune system and, as a result, suppress the fungal infection."
More about the study
The study was performed using lung samples of 169 patients with influenza or COVID-19, with or without aspergillosis. Most of the samples were collected over the last couple of years via bronchoalveolar lavage, a classical diagnostic technique for suspected lung infections, and stored in the Leuven biobank.
In 2018, Professor Joost Wauters and his team were the first to report the dangerous combination of aspergillosis and influenza, which led to worldwide vigilance in intensive care units. The current follow-up study now uncovers the mechanism, which will pave the way for the development of biomarkers and modified treatments for patients with this double infection. The corona pandemic made it possible to include the samples of patients with COVID-19 as well as samples of patients with influenza.
More information: Simon Feys et al, Lung epithelial and myeloid innate immunity in influenza-associated or COVID-19-associated pulmonary aspergillosis: an observational study, The Lancet Respiratory Medicine (2022). DOI: 10.1016/S2213-2600(22)00259-4



















