This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Unraveling the genetic factors behind faulty insulin secretion
A study of the genetic variations that underlie differences in insulin secretion in mice has identified a number of candidate genes that may drive the development of conditions such as type 2 diabetes.
The study, published today as an eLife Reviewed Preprint, offers what the editors describe as a fundamental resource detailing the variations in calcium ion oscillations in the islet cells that comprise part of the endocrine pancreas, namely beta cells, which in turn secrete insulin. The editors describe the strength of evidence as compelling, with strong support from results from human genome-wide association studies (GWAS).
These data have also been used to craft a streamlined, user-friendly web interface that is publicly available, allowing further study into potential genes of interest in islet cell function.
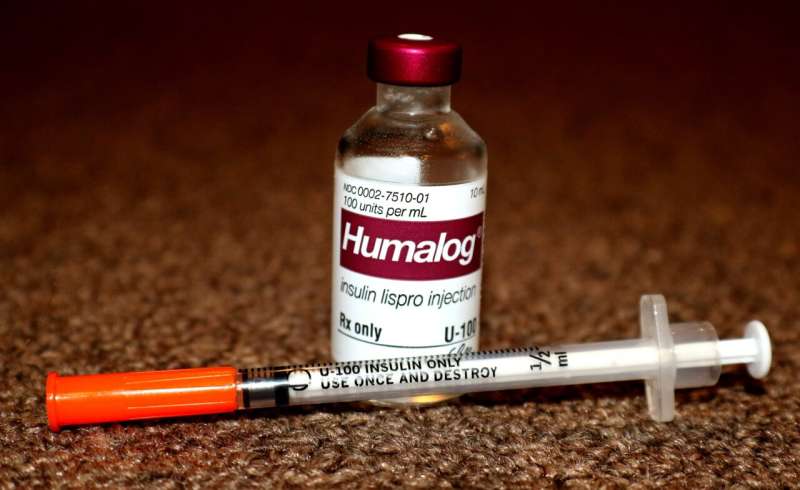
Type 2 diabetes arises when the beta cells of the pancreas do not secrete enough insulin to meet the body's metabolic demands. Insulin resistance, usually evoked by obesity, increases the demand for insulin. Under these conditions, genetic variation in the capacity for insulin secretion can create a bottleneck leading to insufficient insulin. For this reason, the majority of mutations responsible for susceptibility to type 2 diabetes affect genes involved in beta cell function.
The release of insulin from beta cells is brought about by an influx of calcium ions to the beta cells. Pancreatic beta cells are nutrient-sensors—in response to nutrient stimuli, such as glucose, the beta cells set off a chain of events that lead to an influx of calcium ions that triggers the release of insulin. To characterize the genetic factors underlying improper insulin secretion, the team surveyed calcium ion dynamics across eight genetically diverse mouse strains—founder mouse strains from the Collaborative Cross panel and the Diversity Outbred stock.
"Using genetically diverse mice allows us to more closely mimic the human population and identify genetic drivers of disease," says co-lead author Lauren Clark, a Graduate Student in the Department of Biochemistry, University of Wisconsin-Madison, Wisconsin, US. Clark served as co-lead author of the study alongside Christopher Emfinger, a Postdoctoral fellow in the Department of Biochemistry, University of Wisconsin-Madison.
Clark, Emfinger and colleagues selected various stimulatory conditions to allow them to assess the calcium ion dynamics in response to different nutrient stimuli across the eight founder mouse strains.
The team used an analytical technique called unsupervised clustering to highlight groups of proteins that showed a strong positive or negative correlation to a particular calcium ion response. In total, they assessed 4054 proteins, and found that 363 strongly correlated to multiple processes that affected calcium ion dynamics, and thus the secretion of insulin. Notably, a number of these proteins had previously been shown to function in the pancreas islet cells, including PCSK1, SUR1 and GLUT2.
However, this finding only provided correlation between the abundance of islet proteins and the patterns of calcium oscillations—the team could not say for sure if a particular protein caused the changes, or was a consequence of the changes. In order to disentangle cause from consequence, and establish the relevance to humans, the team looked at the equivalent human genes (orthologues) that encode the identified proteins.
They sought to determine whether these orthologous genes served a role in diabetes susceptibility. Using human GWAS, they found that many of these genes had nearby single nucleotide polymorphisms (SNP) linked to blood glucose and insulin. While not definitive, filtering the candidate proteins for islet cell associations in human GWAS suggests a likely causal role in mediating calcium ion dynamics and insulin secretion.
In total, integrating the human GWAS data with the candidate proteins identified around 650 genes with glycemic SNPs and correlation to at least one calcium oscillation parameter, of which around one-third had previously been shown to have a role in islet function. These included well established drivers of insulin secretion; SUR1, GLUT2 and GNAS.
In addition to identifying candidate proteins with a regulatory role in calcium ion dynamics and insulin secretion, the authors created a user-friendly web interface to enable researchers to better identify proteins involved in beta cell function. "Our findings will extend beyond the mouse strains we studied here. Our resource will enable other labs to explore novel roles in islets for their proteins of interest," says Chris Emfinger.
The study will be included in eLife's upcoming Special Issue on systems genetics.
More information: Christopher H. Emfinger et al, Novel regulators of islet function identified from genetic variation in mouse islet Ca2+ oscillations, eLife (2023). DOI: 10.7554/eLife.88189.1


















