Novel mechanisms underlying major childhood neuromuscular disease identified
A study by scientists from the Motor Neuron Center at Columbia University Medical Center (CUMC) suggests that spinal muscular atrophy (SMA), a genetic neuromuscular disease in infants and children, results primarily from motor circuit dysfunction, not motor neuron or muscle cell dysfunction, as is commonly thought. In a second study, the researchers identified the molecular pathway in SMA that leads to problems with motor function. Findings from the studies, conducted in fruit fly, zebrafish and mouse models of SMA, could lead to therapies for this debilitating and often fatal neuromuscular disease. Both studies were published today in the online edition of the journal Cell.
"Scientists call SMA a motor neuron disease, and there is post-mortem evidence that it does cause motor neurons to die," said Brian McCabe, PhD, assistant professor of pathology and cell biology and of neuroscience in the Motor Neuron Center, who led the first study. "However, it was not clear whether the death of motor neurons is a cause of the disease or an effect. Our findings in the fruit fly SMA model show that the disease originates in other motor circuit neurons, which then causes motor neurons to malfunction."
In motor circuits, which coordinate muscle movement, specialized sensory neurons called proprioceptive neurons pick up and relay information to the spinal cord and brain about the body's position in space. The central nervous system then processes and relays the signals, including via interneurons, to motor neurons, which in turn stimulate muscle movement.
"To our knowledge, this is the first clear demonstration in a model organism that defects in the function of a neuronal circuit are the cause of a neurological disease," added Dr. McCabe.
SMA is a hereditary neuromuscular disease characterized by muscle atrophy and weakness. The disease is caused by defects in a gene called SMN1 (survival motor neuron 1), which encodes the SMN protein. There are several forms of SMA, distinguished by time of onset and clinical severity. The most severe form, Type 1, appears before six months of age and generally results in death by age two. In milder forms, symptoms may not appear until much later in childhood or even in early adulthood. There is no treatment for SMA, which is estimated to affect as many as 10,000 to 25,000 children and adults in the United States and is the leading genetic cause of death in infants.
To study the cause of SMA, the researchers worked with fruit flies that had been genetically altered so that every cell had a defective copy of the SMN1 gene. The flies' cells contained low levels of SMN protein, resulting in reduced muscle size and motor function, much as in humans with SMA. When fully functional copies of SMN1 were introduced into the flies' motor neurons or muscle cells, the cell types previously thought to be affected, the flies unexpectedly showed no improvement. Only when SMN1 was returned to other motor circuit neurons—in particular, proprioceptive neurons and interneurons—were muscle size and motor function restored.
In further experiments, the researchers demonstrated that in fruit flies with defective SMN1, proprioceptive neurons and interneurons do not produce enough neurotransmitters. When the flies' potassium channels were genetically blocked—thereby increasing neurotransmitter output—muscle size and motor function improved. The same effect was seen when the flies were given drugs that block potassium channels, suggesting that this class of drugs might help patients with SMA.
Supported by these findings, in July, the SMA Clinical Research Center at CUMC launched a clinical trial of a potassium channel blocker called dalfampridine (Ampyra) for the treatment of patients with SMA. The study will assess whether the drug improves walking ability and endurance in adults with SMA Type 3, compared with placebo. Claudia A. Chiriboga, MD, MPH, associate professor of Clinical Neurology at CUMC, is the lead clinical investigator. Ampyra was approved by the FDA for the treatment of patients with multiple sclerosis in 2010.
"This drug is unlikely to be a cure for SMA, but we hope it will benefit patient symptoms," said Dr. McCabe. "Other compounds at various stages of development hold promise to fix the underlying molecular problem."
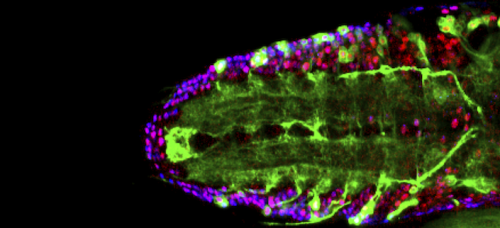
The second study, led jointly by Livio Pellizzoni, PhD, assistant professor of Pathology and Cell Biology in the Motor Neuron Center, and Dr. McCabe, sought to determine how the loss of SMN protein—which is expressed in all cells—leads to the selective disruption of motor circuits. Working with models of SMA in mammalian cells, fruit flies, zebrafish, and mice, the researchers demonstrated that SMN1 deficiency disrupts a fundamental cellular process known as RNA splicing with detrimental effects on the expression of a subset of genes that contain a rare type of intron. (In the process of RNA splicing, parts of RNA called introns are removed so a gene can be translated into protein.) By studying the function of this group of genes affected by the loss of SMN1, the researchers discovered a novel gene—which they named stasimon—that is critically required for motor circuit activity in vivo. They further showed that restoring expression of stasimon was alone sufficient to correct key aspects of motor dysfunction in both invertebrate and vertebrate models of SMA.
"What is intriguing about SMA is that mutations in the disease gene SMN1 reduce its expression in all cells, yet patients get this specific disease of the motor system. The reason for this has been a longstanding enigma in the SMA field," said Dr. Pellizzoni. "Our findings provide the first explanation at the molecular level as to how this can happen. We show a direct link from the loss of the SMN1 gene to defective splicing of a critical neuronal gene to motor circuit dysfunction, establishing SMA as a disease of RNA splicing. By linking SMN-dependent splicing events to motor circuit function, our work has implications for understanding the pathogenic mechanisms not only of SMA, but also of other neurological disorders," said Dr. Pellizzoni.
"The potential added value of our study is that we've identified a novel gene that is targeted by the disease protein. When disrupted, this gene—stasimon—appears to contribute to the development of SMA in model organisms. The implication is that this gene and the pathway in which it functions might be new candidate therapeutic targets," Dr. Pellizzoni added.
More information: The first paper is titled, "SMN is required for sensory-motor circuit function in Drosophila." The second paper is titled, "A SMN-Dependent U12 Splicing Event Essential for Motor Circuit Function."















