Evolution in the antibody factory: How immune cells are able to advance their own evolution
Immune system B cells play a crucial role in the defence of pathogens; when they detect such an intruder, they produce antibodies that help to combat the enemy. They concurrently and continuously improve these molecules to more precisely recognize the pathogens. A team of scientists with participation of the Helmholtz Centre for Infection Research (HZI) has discovered that during this process the cells are able to advance their own evolution themselves by increasing the selection pressure through previously-produced antibodies. The results are also significant for the development of new vaccination strategies.
The principle of evolution signifies the competition for limited resources and a reaction to changeable environmental conditions. This selection pressure is virtually produced by the B cells on their own; they subject themselves to an optimization cycle in the lymph node, a process which only a few of them survive, i.e. particular cells that are able to produce "better" antibody molecules as compared to those that already exist within the body. The quality of these antibodies is tested in the lymph nodes, and only those cells that are able to prove themselves here receive signals from other immune cells that assure their survival.
Every B cell carries a specific defence molecule on its surface. It recognizes certain structures of pathogens – so-called antigens – similar to the way a key fits into one specific lock. This molecule is furthermore produced in a certain form that does not remain on the cell surface; rather, it travels with blood and lymph throughout the body. If the antibody encounters an antigen, it either binds it to neutralise it, or it sends out an alarm to other players within the immune system.
At the beginning of an infection there are, figuratively speaking, several keys that do not yet fit properly. This changes in the course of a process that immunologists refer to as "somatic hypermutation": B cells mutate those gene segments that determine the design of both the surface molecule and the soluble variation – thus influencing how strongly the antibodies attach themselves to the pathogens. Those cells, in which the optimal fit of the key increases, survive and multiply. They then produce the desired molecule in large quantities and thus help us to get healthy again.
But how do the immune cells know that they are on the right way with this arbitrary mutation process, i.e. that the key will fit better later on? Scientists from England, Germany and Switzerland have now been able to answer this question jointly in a collaborative project between Dr. Kai-Michael Toellner, University of Birmingham, and Prof. Michael Meyer-Hermann, Head of the Department Systems Immunology. They published their findings in the renowned Journal of Experimental Medicine. Meyer-Hermann makes use of mathematical models to understand diseases more thoroughly and quicker. "Systems immunology enables us to simulate, in a short amount of time, numerous experimental conditions," he describes his area of expertise. With the aid of such mathematical simulations followed by experimental examinations, the researchers discovered that the antibody producers advance their own evolution, which represents without a doubt an alignment with the enormous selection pressure that we are subject to due to a constant threat from pathogens.
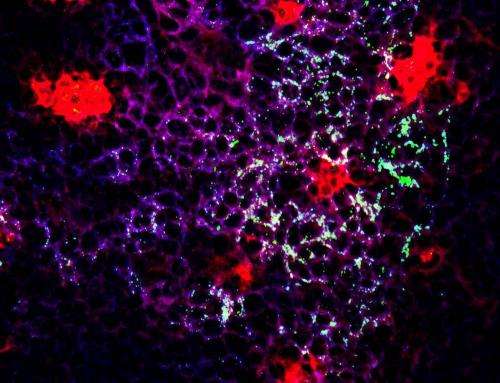
The stage for this process is the so-called germinal centres within the lymph nodes. Here, the maturing B cells encounter the antigens. The researchers' results suggest that completed antibodies from all germinal centres re-appear at the sites of antibody production and bind there to pathogen fragments as well. They represent competition thereby for those cells that are still in the process of refining the optimal fit of their surface molecules. Once the immune cells with their "surface-key" are able to bind to the "antigen locks" more readily than the finished antibodies, they receive survival signals and their key-form asserts itself.
"This is the 'survival of the fittest' as previously described by Charles Darwin on a molecular level," compares Meyer-Hermann. Studies with mice were able to be confirmed in computer simulations only under the assumption that the B cells compete with their own products – namely the antibodies – for the right to bind to antigens.
This astounding mechanism could, in the future, improve conventional vaccination methods. "It is plausible that patients could be administered, in addition to a vaccine, sufficiently-strong-binding antibodies," explains Meyer-Hermann. "Our models constructed in the computer suggest that this method accelerates the process of identifying optimal antibodies." The scientists suspect that the addition of antibodies manipulates the reaction to vaccination, since the newly-generated antibodies are now in competition with the externally-introduced molecules. The conditions for selection are thus intensified and the B cells react by producing optimal antibodies earlier on. The result is that vaccinations could take effect quicker.
More information: Yang Zhang, Michael Meyer-Hermann, Laura A. George, Marc Thilo Figge, Mahmood Khan, Margaret Goodall, Stephen P. Young, Adam Reynolds, Francesco Falciani, Ari Waisman, Clare A. Notley, Michael R. Ehrenstein, Marie Kosco-Vilbois and Kai-Michael Toellner, Germinal center B cells govern their own fate via antibody feedback Journal of Experimental Medicine, 2013, doi: 10.1084/jem.20120150













