Low cholesterol in immune cells tied to slow progression of HIV
People infected with HIV whose immune cells have low cholesterol levels experience much slower disease progression, even without medication, according to University of Pittsburgh Graduate School of Public Health research that could lead to new strategies to control infection.
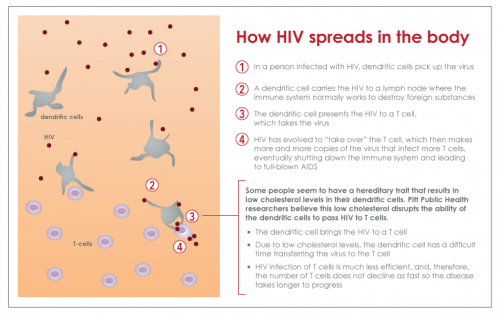
The Pitt Public Health researchers found that low cholesterol in certain cells, which is likely an inherited trait, affects the ability of the body to transmit the virus to other cells. The discovery, funded by the National Institutes of Health (NIH), is featured in today's issue of mBio, the journal of the American Society for Microbiology.
When HIV enters the body, it is typically picked up by immune system cells called dendritic cells, which recognize foreign agents and transport the virus to lymph nodes where it is passed to other immune system cells, including T cells. HIV then uses T cells as its main site of replication. It is through this mechanism that levels of HIV increase and overwhelm the immune system, leading to AIDS. Once a person develops AIDS, the body can no longer fight infections and cancers. Prior to effective drug therapy, the person died within one to two years after the AIDS diagnosis.
"We've known for two decades that some people don't have the dramatic loss in their T cells and progression to AIDS that you'd expect without drug therapy," said lead author Giovanna Rappocciolo, Ph.D., an assistant professor at Pitt Public Health. "Instead the disease is much slower to progress, and we believe low cholesterol in dendritic cells may be a reason."
The discovery was made possible by using 30 years of data and biologic specimens collected through the Pitt Men's Study, a confidential research study of the natural history of HIV/AIDS, part of the national NIH-funded Multicenter AIDS Cohort Study (MACS).
"We couldn't have made this discovery without the MACS. Results like ours are the real pay-off of the past three decades of meticulous data and specimen collection," said senior author Charles Rinaldo, Ph.D., chairman of Pitt Public Health's Department of Infectious Diseases and Microbiology, and professor of pathology. "It is thanks to our dedicated volunteer participants that we are making such important advances in understanding HIV, and applying it to preventing and treating AIDS."
Medications called combination antiretroviral therapy (ART) disrupt the viral replication process and can delay the onset of AIDS by decades.
However, even without taking ART, a small percentage of people infected with HIV do not have the persistent loss of T cells and increase in levels of HIV after initial infection. They can sometimes go many years, even more than a decade, without the virus seriously compromising the immune system or leading to AIDS.
Through the Pitt Men's Study/MACS, eight such "nonprogressors" were assessed twice a year for an average of 11 years and compared to eight typically progressing HIV-positive counterparts.
Dr. Rappocciolo and her colleagues found that in nonprogressors, the dendritic cells were not transferring the virus to T cells at detectible levels. When taking a closer look at these dendritic cells, the researchers discovered that the cells had low levels of cholesterol, even though the nonprogressors had regular levels of cholesterol in their blood. A similar finding was shown for B lymphocytes, which also pass HIV to T cells, leading to high rates of HIV replication.
Cholesterol is an essential component of the outer membranes of cells. It is required for HIV to replicate efficiently in different types of cells. None of the study participants were taking statins, which are cholesterol-lowering medications that some people take to prevent vascular problems when cholesterol in their blood is too high.
When HIV was directly mixed with the nonprogressors' T cells in the laboratory, those T cells became infected with the virus at the same rate as the T cells of the regularly progressing, HIV-positive participants. Indeed, T cells from the nonprogressors had normal levels of cholesterol.
"This means that the disruption is unlikely to be due to a problem with the T cells, further supporting our conclusion that the slow progression is linked to low cholesterol in the dendritic cells and B cells," said Dr. Rappocciolo.
"What is most intriguing is that dendritic cells in the nonprogressors had this protective trait years before they became infected with HIV," Dr. Rinaldo said. "This strongly suggests that the inability of their dendritic cells and B cells to pass HIV to their T cells is a protective trait genetically inherited by a small percentage of people. Understanding how this works could be an important clue in developing new approaches to prevent progression of HIV infection."

















