Protein that activates immune response harms body's ability to fight HIV
In findings they call counterintuitive, a team of UCLA-led researchers suggests that blocking a protein, which is crucial to initiating the immune response against viral infections, may actually help combat HIV.
Findings from a study in animals appear to demonstrate that temporarily blocking a type of protein, called type I interferon, can restore immune function and speed up viral suppression during treatment with anti-viral drugs for people with chronic infection of the virus that causes AIDS.
This is the first study to show the role that type I interferon plays in driving the body's immune destruction during HIV infection, said Scott Kitchen, associate professor of medicine in the division of hematology/oncology at the David Geffen School of Medicine at UCLA and senior author of the study published in the peer-reviewed Journal of Clinical Investigation.
"This finding is completely counterintuitive, because many believe that the more interferon at work, the better," said Kitchen, a member of the UCLA AIDS Institute. "We show that the type of interferon being produced during chronic stages of HIV infection has detrimental effects on the body's ability to fight off HIV and other types of infection or cancer and could actually be contributing to accelerated HIV disease."
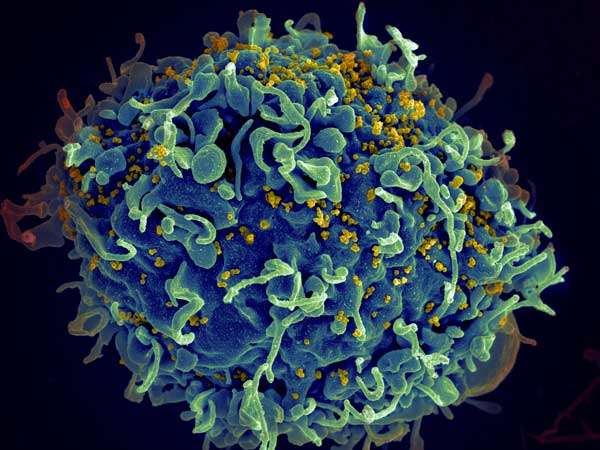
HIV cripples the immune system by destroying immune cells called CD4 T cells, which are activated during early HIV infection by type I interferon. CD4 T cells are also known as "helper" cells because they signal another type of T cell, the CD8, to destroy HIV-infected cells. Also, HIV evades the body's CD8 cells by constantly mutating, escaping recognition by CD8 cells and making them ineffective. The chronically heightened state of inflammation and activation eventually leads to what is known as immune exhaustion when the immune cells can no longer function properly to clear infected cells. This, along with the loss of CD4 T cells ultimately leads to the destruction of the immune system.
The researchers' idea is to block type I interferon to reduce chronic activation of the immune cells, which could give the exhausted CD8 T cells the opportunity to restore their abilities to fighting strength. Combine that with antiretroviral therapy and it may be possible to both restore immune function and eradicate HIV throughout the body.The researchers used "humanized mice," which have had their immune systems replaced with human immune system cells, thymus tissue and bone marrow. They treated HIV-infected mice with antibodies that blocked type I interferons, which allowed the mice's immune systems to revert from the state of exhaustion. This made it possible for their immune systems to produce sufficient amounts of CD8 T cells that were primed to attack and kill HIV-infected cells. When combined with antiretroviral therapy, the treatment accelerated the effect of antiretroviral therapy in suppressing HIV.
"We found—counterintuitively—that blocking this immune response against the virus had beneficial effects in lowering the amounts of virus and increasing the ability of the immune response to clear out the virus," said Kitchen, who is also director of the UCLA Humanized Mouse Core Laboratory.
Kitchen noted that these findings offer a proof of principle in a humanized mouse system and are not definitive. More experiments are needed in non-human primates before moving on to human clinical trials to determine whether the researchers' theory holds up and this treatment is safe in humans.
But the findings offer a new perspective into the function of type I interferon during untreated and treated HIV chronic infection, said Anjie Zhen, a postdoctoral scholar and member of the UCLA AIDS Institute who led the study.
"This could have profound implications for the development of therapies that include such approaches as interferon alpha therapy," Zhen said. "This shows that a proper balance is required when administering this type of therapy, where too much can have detrimental effects in suppressing important immune responses."
More information: Anjie Zhen et al. Targeting type I interferon–mediated activation restores immune function in chronic HIV infection, Journal of Clinical Investigation (2016). DOI: 10.1172/JCI89488



















