How rogue immune cells cross the blood-brain barrier to cause multiple sclerosis
Drug designers working on therapeutics against multiple sclerosis should focus on blocking two distinct ways rogue immune cells attack healthy neurons, according to a new study in the journal Cell Reports.
In multiple sclerosis, immune cells degrade the insulation that protects neurons and allows them to signal to one another, but little is known about how immune cells penetrate the blood-brain barrier to get to neurons. Researchers led by Sarah Lutz, University of Illinois at Chicago College of Medicine while she was a post-doctoral fellow of Dritan Agalliu at Columbia University; and Sunil Gandhi, University of California, Irvine, have uncovered two different ways immune cells gain access to neurons and wreak their havoc.
Multiple sclerosis is a neurodegenerative inflammatory disease that affects approximately 2.5 million people worldwide. Immune cells turn against the body and cause damage to the myelin sheath, which encases neurons like the insulation on a wire. Loss of myelin interferes with the transmission of signals along the nerve fibers and impairs motor function, including walking and speech. Symptoms, which can be sporadic or progressive, range from mild to debilitating.
While researchers have known that two different kinds of immune cells, Th1 and Th17 lymphocytes, are involved in degrading myelin around neurons in multiple sclerosis, they didn't know exactly how these cells crossed the blood-brain barrier to access neurons.
The blood-brain barrier is a bit of a misnomer. It not only protects the brain, but also the spine, and refers to the fact that blood vessels that supply the brain and spine are virtually impermeable because the cells that make up those blood vessels—called endothelial cells—are bolted tightly together by protein complexes called tight junctions. This prevents certain chemicals, harmful microbes and cells that circulate in the blood from gaining access to the brain and spine. In blood vessels that supply other organs of the body, endothelial cells are more loosely bound to one another and the connections can be adjusted to allow for the exchange of molecules and cells from the bloodstream into tissues and vice versa.
"In autoimmune diseases like multiple sclerosis, immune cells that enter the brain and spinal cord cause disease," said Lutz, assistant professor of anatomy and cell biology in the UIC College of Medicine and the lead author of the paper. "A better understanding of how these cells cross the blood-brain barrier will aid our efforts to develop specific therapies to keep them out."
To explore how Th1 and Th17 immune cells gain access to neurons in multiple sclerosis, Lutz and her colleagues looked at the blood-brain barrier in mice with experimental autoimmune encephalomyelitis—a mouse version of multiple sclerosis.
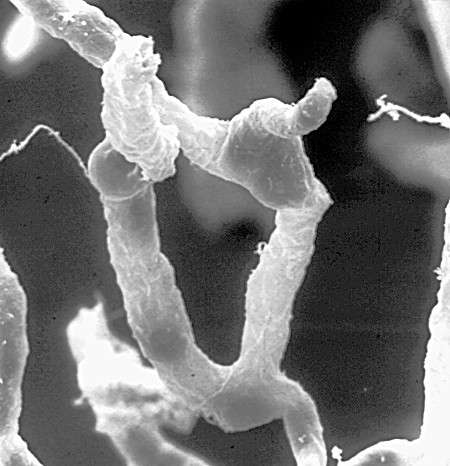
They genetically labeled blood vessel endothelial cell tight junctions with a fluorescent protein to examine if and how tight junctions are involved in autoimmune encephalomyelitis in vivo in their mice. The researchers observed that the tight junctions were significantly deteriorated in the presence of Th17 cells, and that this took place early in the onset of disease. Approximately three days later in the disease process, Lutz and colleagues found that Th1 cells were accessing and degrading myelin and neurons—but these cells did not pass through tight junctions like the Th17 cells did. Instead, the circulating Th1 cells got to neurons by going through the blood vessel endothelial cells using specialized cell membrane structures called caveolae. Caveolae are small pits or "caves" found on the surface of many cell types and help facilitate the passage of various molecules and cells into and/or through cells. In mice with autoimmune encephalomyelitis bred to lack caveolae, the researchers found almost no Th1 cells in the brain and spinal cord. They determined that caveolae on endothelial cells that make up blood vessels are required to help ferry Th1 cells through the blood-brain barrier.
"This is the first time we have ever seen, in live animals in real-time, the different means by which these two cell types gain access to myelin and nerves," said Lutz. "Now that we know how these cells get to neurons, drugs or small molecules can be designed that interfere with or block each of these processes to help treat and possibly prevent multiple sclerosis."
Dae Hwan Kim, Carl V. L. Olson, Kyle Ellefsen, and Jennifer Bates, University of California, Irvine; and Julian Smith, Columbia University Medical Center, New York, are co-authors on the paper.
More information: Cell Reports (2017). DOI: 10.1016/j.celrep.2017.10.094 , www.cell.com/cell-reports/full … 2211-1247(17)31574-7



















