Researchers identify renegade cells that portend relapse in children with leukemia
Researchers at the Stanford University School of Medicine have developed a technique that allowed them to determine at diagnosis whether children with acute lymphoblastic leukemia would relapse following treatment.
The method, described in a paper publishing online March 5 in Nature Medicine, predicted relapse in the cohort they examined with 85 percent accuracy, a significant improvement from 66 percent accuracy achieved by the current risk stratification method used at diagnosis. The method examines cancer cells one at a time using mass cytometry, a technique developed by Garry Nolan, PhD, professor of microbiology and immunology and a senior author of the study. Using data on the cells' stage of development and signaling behavior, the scientists figured out how to identify a tiny subset of malignant cells that, if present, predisposed a patient to relapse.
Called the Developmentally Dependent Predictor of Relapse, the technique could help identify which acute lymphoblastic leukemia patients need a different approach to cancer treatment, and may provide good clues about how to find new drugs to target the deadliest cancer cells, the researchers said.
"We really need to personalize treatment to leukemia patients better than we do now," said graduate student Zinaida Good, the study's co-lead author. "There is a lot of room for improvement here. This study makes a contribution to our ability to stratify patients better and not treat everybody the same way."
Postdoctoral scholar Jolanda Sarno, PhD, is the other lead author.
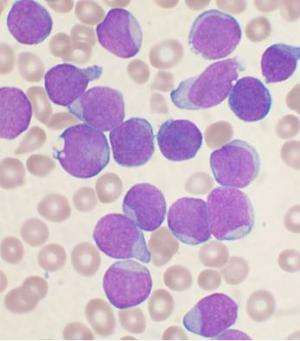
Pediatric acute lymphoblastic leukemia is the most common childhood cancer, diagnosed in about 3,000 American children per year. The study focused on the most frequently found type of the disease, called B-cell precursor ALL, which occurs when certain white blood cells take a wrong turn during development and become malignant. Although the majority of cases are cured with existing chemotherapy drugs, 10-20 percent of patients relapse. Among those who relapse, about 40-80 percent die of their disease within five years.
"Acute lymphoblastic leukemia is a very well-characterized cancer that has a robust risk prediction measure already, but the final risk of relapse is usually not known until a few months into treatment, and there are still patients who get missed," said Kara Davis, DO, assistant professor of pediatric hematology and oncology and the other senior author of the study. "And, with existing prediction tools, when we do identify someone as high-risk for relapse, we don't know what it is about their leukemia that raises their risk."
A few really bad apples
Prior research strongly suggested that cancer relapse may be driven by a few treatment-resistant cells that are present from the beginning of the disease. "We wondered, can we identify those cells at the time the patient first presents to clinic, and can we treat patients with a specific therpy to target them?" Davis said.
Using mass cytometry, the researchers tested bone marrow samples taken from 60 ALL patients at the time of their diagnosis. Each patient had three to 15 years of follow-up medical records available for analysis, including information on whether they had relapsed.
To identify the problematic cells from among the millions of cells in each sample, the researchers had to figure out how to organize the data. "Every patient has vastly different features to their cancer, and we had to ask, 'Is there any common thread between them?'" Davis said.
The solution, the team found, was to compare leukemic cells to their most similar normal cells along the trajectory of healthy B-cell development. Of 15 developmental cell stages examined, malignant cells arising from just two adjacent stages in B-cell maturation—the pro-B2 and pre-B1 stages—were the bad actors: If these particular types of malignant cells had certain signaling behavior at diagnosis, patients were almost certain to relapse after standard chemotherapy.
"Stem cell biology is evolving, and we've learned a lot about how normal development takes place," Good said. "Now we can use that to understand cancer better."
Combining methods gets better results
When the new method for predicting relapse was combined with existing methods based on patients' early response to treatment, the results were better than those obtained by either method alone.
"We do not understand the mechanisms by which malignant cells from the pro-B2 and pre-B1 stages of development resist treatment," Davis said, adding that the team has begun looking for existing drugs to target them.
They plan to validate their method in a larger number of patients and to evaluate whether the same general approach could predict relapse in other forms of cancer. Further, since the method provides information about treatment-resistant cells, patients found to be at high risk for relapse could benefit from treatments specific to those cells.
"We think that being more precise in risk prediction could benefit patients at both low and high risk for relapse," Davis said.
The study is an example of Stanford Medicine's focus on precision health, the goal of which is to anticipate and prevent disease in the healthy and precisely diagnose and treat disease in the ill.
More information: Single-cell developmental classification of B cell precursor acute lymphoblastic leukemia at diagnosis reveals predictors of relapse, Nature Medicine (2018). nature.com/articles/doi:10.1038/nm.4505


















