Second 'don't eat me' signal found on cancer cells
A second biological pathway that signals immune cells not to engulf and kill cancer cells has been identified by researchers at the Stanford University School of Medicine.
An antibody that blocks the "don't eat me" signal has shown promise as a cancer treatment in animal models and is currently in clinical trials. Combining that antibody, known as anti-CD47, with another that blocks this newly discovered pathway could further enhance the ability of the immune system to eradicate many types of cancers, the researchers believe.
"The development of cancer cells triggers the generation of SOS molecules recognized by the body's scavenger cells, called macrophages," said Irving Weissman, MD, the director of Stanford's Institute for Stem Cell Biology and Regenerative Medicine, and also of its Ludwig Cancer Center. "However, aggressive cancers express a 'don't eat me' signal in the form of CD47 on their surfaces. Now we've identified a second 'don't eat me' signal and its complementary receptor on macrophages. We've also shown that we can overcome this signal with specific antibodies and restore the ability of macrophages to kill the cancer cells."
A paper describing the findings will be published online Nov. 27 in Nature Immunology. Weissman, a professor of pathology and of developmental biology, shares senior authorship of the study with former postdoctoral scholar Roy Maute, PhD, who is now head of biology at Ab Initio Biotherapeutics Inc. Graduate student Amira Barkal shares lead authorship with former graduate student Kipp Weiskopf, MD, PhD, who is now a resident at Brigham and Women's Hospital.
"Simultaneously blocking both these pathways in mice resulted in the infiltration of the tumor with many types of immune cells and significantly promoted tumor clearance, resulting in smaller tumors overall," Barkal said. "We are excited about the possibility of a double- or perhaps even triple-pronged therapy in humans in which we combine multiple blockades to cancer growth."
Importance of macrophages
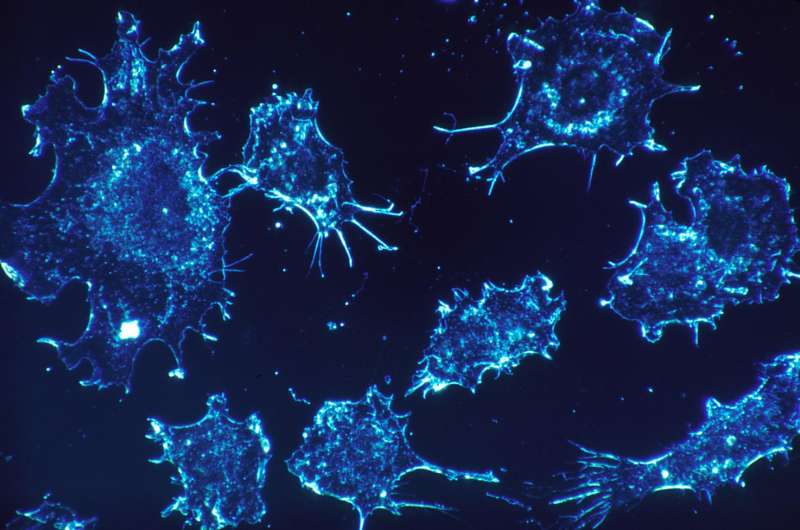
Macrophages are large white blood cells found in nearly all the body's tissues. As part of what's known as the innate immune system, they engulf and kill foreign invaders like bacteria or viruses. They also destroy dead and dying cells and, in some cases, cancer cells whose internal development cues have gone haywire.
The "don't eat me" signal was identified in Weissman's laboratory in 2009. His team found that nearly all cancer cells express high levels of a molecule called CD47 on their surfaces. They showed that CD47 binds to a protein called SIRPalpha on the surface of macrophages, inhibiting their ability to kill the cancer cells.
Animal studies showed that treatment with an anti-CD47 antibody vastly improved the ability of macrophages to kill cancer cells and even led to some cures in mouse models of cancer. Phase-1 clinical trials are currently underway at Stanford and in the United Kingdom to test the safety and efficacy of the treatment in humans with a variety of blood and solid tumors.
The newly discovered binding interaction used by cancer cells to evade macrophages capitalizes on a protein structure on the cancer cells' surface called the major histocompatibility complex class 1, or MHC class 1. Human tumors that have high levels of MHC class 1 on their surfaces are more resistant to anti-CD47 treatment than are those with lower levels of the complex, the researchers found.
Component of adaptive immunity
MHC class 1 is an important component of adaptive immunity, the second major arm of the immune system, which relies on immune cells called T cells and B cells to nimbly and specifically respond to foreign invaders and cell damage. Most cells of the body express MHC class 1 on their surfaces as a way to indiscriminately display bits of many proteins found within the cell—a kind of random sampling of a cell's innards that provides a window into its health and function. If the protein bits, called peptides, displayed by the MHC are abnormal, a T cell destroys the cell. Although the relationship between MHC class 1 and T cells has been well-established, it's been unclear whether and how the complex interacts with macrophages.
Barkal and her colleagues found that a protein called LILRB1 on the surface of macrophages binds to a portion of MHC class 1 on cancer cells that is widely shared across individuals. This binding inhibits the ability of macrophages to engulf and kill the cancer cells, both when growing in a laboratory dish and in mice with human tumors, the researchers found. Inhibiting both the CD47-mediated pathway and the LILRB1 pathway significantly slowed tumor growth in mice.
Understanding the balance between adaptive and innate immunity is important in cancer immunotherapy. For example, it's not uncommon for human cancer cells to reduce the levels of MHC class 1 on their surfaces to escape destruction by T cells. People with these types of tumors may be poor candidates for cancer immunotherapies meant to stimulate T cell activity against the cancer. But these cells may then be particularly vulnerable to anti-CD47 treatment, the researchers believe. Conversely, cancer cells with robust MHC class 1 on their surfaces may be less susceptible to anti-CD47.
"In some cancers, MHC class 1 expression, for a variety of reasons, is not reduced," Weissman said, "and this helps the cancer cells escape from macrophages. These findings help us understand the many ways cancer cells can evade macrophages, and how we might block these escape pathways."
"The fact that there are at least two redundant mechanisms to modulate macrophage activity is a testament to how critically important it is to tightly control our immune responses," Barkal said. "It's possible that future studies will identify even more of these pathways, which will give us additional targets for cancer immunotherapy."
More information: Engagement of MHC class I by the inhibitory receptor LILRB1 suppresses macrophages and is a target of cancer immunotherapy, Nature Immunology (2017). nature.com/articles/doi:10.1038/s41590-017-0004-z




















